7. DISEASE MANAGEMENT
7.1. Neoadjuvant therapy
7.1.1. Introduction
The standard treatment for patients with urothelial MIBC and MIBC with variant histologies is RC. However, RC only provides 5-year survival in about 50% of patients [246-250]. To improve survival in patients with cN0M0 disease, cisplatin-based NAC has been used since the 1980s [246-252].
7.1.2. Role of cisplatin-based chemotherapy
There are theoretical advantages and disadvantages of administering chemotherapy before planned definitive surgery to patients with resectable muscle-invasive cN0M0 UC of the bladder:
- Chemotherapy is delivered at the earliest time-point, when the burden of micrometastatic disease is expected to be low.
- Potential reflection of in-vivo chemosensitivity.
- Tolerability of chemotherapy and patient compliance are expected to be better pre-cystectomy.
- Patients may respond to NAC and have a favourable pathological response as determined mainly by achieving ypT0, < ypT1, ypN0 and negative surgical margins. A recently reported analysis to identify the optimal definition of pathological response reported a significantly higher risk of recurrence in patients with ypTaN0 or ypT1N0 disease (with or without Tis) at RC and thus proposed that optimal pathological response after NAC be defined as attainment of ypT0N0/ypTisN0 at RC [253].
- Delayed cystectomy might compromise the outcome in patients not sensitive to chemotherapy [254-256].
A comparative survival analysis of patients treated with NAC and RC vs. RC alone based on data from the U.S. National Cancer Database showed that organ-confined disease (< pT2) after NAC was associated with decreased risk of death (HR: 0.85, 95% CI: 0.79–0.91) compared to RC alone, whereas > pT2 was associated with increased risk of death (HR: 1.46, 95% CI: 1.34–1.60) [257]. However, there are no prospective trials indicating that delayed surgery due to NAC has a negative impact on survival. In the phase III VESPER trial, comparing gemcitabine/cisplatin (GC) vs. high-dose-intensity methotrexate, vinblastine, doxorubicine and cisplatin (HD-MVAC) in the peri-operative setting, approximately 90% of patients proceeded to surgery (with median delay of 48 days for GC and 51 days for dd-MVAC) [258]. - Neoadjuvant chemotherapy does not seem to affect the outcome of surgical morbidity. In one randomised trial the same distribution of grade 3–4 post-operative complications was seen in both treatment arms [259]. In the combined Nordic trials (n = 620), NAC did not have a major adverse effect on the percentage of performable cystectomies. The cystectomy frequency was 86% in the experimental arm and 87% in the control arm with 71% of patients receiving all three chemotherapy cycles [260].
- Clinical staging using bimanual palpation, CT or MRI may result in over- and understaging and have a staging accuracy of only 70% [88]. Overtreatment is a possible negative consequence.
- Gender may have an impact on chemotherapeutic response and oncologic outcomes [261,262]. Female patients tend to have a better cancer-related response to NAC as compared to male patients.
- Neoadjuvant chemotherapy should only be used in patients eligible for cisplatin-combination chemotherapy; other combinations (or monotherapies) are inferior in metastatic BC and have not been fully tested in a neoadjuvant setting [259,263-271].
7.1.2.1. Summary of available data
Several phase III RCTs addressed the potential survival benefit of NAC administration [259,263-268,272-276]. The main differences in trial designs were the type of chemotherapy (i.e., single-agent cisplatin or combination chemotherapy) and the number of cycles provided. Patients had to be fit for cisplatin. Since these studies differed considerably for patient numbers, patient characteristics (e.g., clinical T-stages included) and the type of definitive treatment offered (cystectomy and/or RT), pooling of results was not possible.
Three meta-analyses were undertaken to establish if NAC prolongs survival [269-271]. In a meta-analysis including updated patient data from 11 randomised trials (n = 3,005), a significant survival benefit was shown in favour of NAC [271]. The most recent meta-analysis included four additional RCTs, and used the updated results from the Nordic I, Nordic II, and BA06 30894 trials including data from 427 new patients and updated information from 1,596 patients. The results of this analysis confirmed the previously published data and showed an 8% absolute improvement in survival at five years with a number needed-to-treat of 12.5 [277]. Only cisplatin-combination chemotherapy with at least one additional chemotherapeutic agent resulted in a meaningful therapeutic benefit [269,271]; the regimens tested were methotrexate, vinblastine, adriamycin (epirubicin) plus cisplatin (MVA(E)C), cisplatin, methotrexate plus vinblastine (CMV), cisplatin plus methotrexate (CM), cisplatin plus adriamycin and cisplatin plus 5-fluorouracil (5-FU) [278].
The updated analysis of a large phase III RCT [263] with a median follow-up of eight years confirmed previous results and provided additional findings:
- 16% reduction in mortality risk;
- improvement in 10-year survival from 30% to 36% with neoadjuvant CMV;
- benefit with regard to distant metastases;
- the addition of neoadjuvant CMV provided no benefit for locoregional control and locoregional DFS, independent of the definitive treatment.
More modern chemotherapeutic regimens such as GC have shown similar pT0/pT1 rates as methotrexate, vinblastine, adriamycin plus cisplatin in retrospective series and pooled data analyses [278-281]. Modified dd-MVAC was tested in two small single-arm phase II studies demonstrating high rates of pathologic complete remission [282,283]. Moreover, a large cross-sectional analysis showed higher rates of down-staging and pathological complete response for dd-MVAC [284].
In the GETUG/AFU V05 VESPER RCT of peri-operative chemotherapy, 500 patients were randomised to either 6 cycles of dd-MVAC once every 2 weeks vs. 4 cycles of GC once every 3 weeks prior to surgery (neoadjuvant group) or after surgery (adjuvant group) with a primary endpoint of progression-free survival (PFS) at 3 years. In 493 patients (437 neoadjuvant and 56 adjuvant), a similar pathologic response rate (ypT0N0) in patients treated with dd-MVAC 42% and GC 36% (p = 0.2) was seen. The < ypT2N0 rate was 63% and 50% in the dd-MVAC and GC patients, respectively. Organ-confined response (< ypT3N0) was observed more frequently in the dd-MVAC arm (77% vs. 63%, p = 0.001). For all patients in the trial, 3-year PFS was improved in the dd-MVAC arm, but the study did not meet its primary endpoint (3-year rate: 64% vs. 56%, HR: 0.77 [95% CI: 0.57–1.02], p = 0.066); nevertheless, the dd-MVAC arm was associated with a significantly longer time to progression (3-year rate: 69% vs. 58%, HR: 0.68 [95% CI: 0.50–0.93], p = 0.014). In the neoadjuvant group, PFS at 3 years was significantly higher in the dd-MVAC arm (66% vs. 56%, HR: 0.70 [95% CI: 0.51–0.96], p = 0.025). Dose-dense MVAC was associated with more severe asthenia and GI side effects than GC [258,285]. Another dose-dense regimen using GC was reported in two small phase II trials [286,287]. While pathological response rates (< pT2) in the range of 45%–57% were achieved, one trial had to be closed prematurely due to high rates of severe vascular events [286]. This approach is therefore not recommended outside of clinical trials.
As an alternative to the standard dose of cisplatin-based NAC with 70 mg/m2 on day 1, split-dose modifications regimens are often used with 35 mg/m2 on days 1+8 or days 1+2. In a retrospective analysis the standard schedule was compared to a split-dose schedule in terms of complete and partial pathological response. A lower number of complete and partial response rates was seen in the split-dose group, but these results were not statistically significant [288].
Efforts aimed at improving the efficacy of NAC in MIBC are ongoing. In the recently reported double-blind, randomised, placebo-controlled, phase II NEOBLADE trial of neoadjuvant gemcitabine and cisplatin chemotherapy with nintedanib, a small molecule inhibitor that targets tyrosine kinases PDGFR, FGFR-1, and VEGFR-2, or placebo, in locally-advanced MIBC, the addition of nintedanib to chemotherapy was safe but did not improve the rate of pathological complete response [289].
There seem to be differences in the outcomes of patients treated with NAC for primary or secondary MIBC with retrospective data suggesting that patients with primary MIBC have better pathologic response rates to NAC in comparison to patients with secondary MIBC [290]. However, in the absence of prospective data, patients with secondary MIBC should be treated similarly to those presenting with primary MIBC [229].
It is unclear, if patients with non-UC histology will also benefit from NAC. A retrospective analysis demonstrated that patients with neuroendocrine tumours had improved OS and lower rates of non-organ-confined disease when receiving neoadjuvant cisplatinum/etoposide chemotherapy. In case of micropapillary differentiation, sarcomatoid differentiation and adenocarcinoma, lower rates of non-organ confined disease were found, but no statistically significant impact on OS. Patients with SCC did not benefit from NAC [291]. A 2019 systematic review showed benefit of NAC for patients with micropapillary-, plasmacytoid-, sarcomatoid-, and mixed variants but especially for patients with neuroendocrine tumours [69]. A U.S. National Cancer Database study evaluating potential associations between receipt of NAC, pathological downstaging and OS for patients with histological subtype MIBC demonstrated that NAC was associated with pathological downstaging for all MIBC histological subtypes (UC; sarcomatoid UC; micropapillary UC; SCC; neuroendocrine carcinoma; and adenocarcinoma), with improved OS for patients with UC, sarcomatoid variant UC and neuroendocrine carcinoma [292].
7.1.3. The role of imaging and predictive biomarkers (see also section 5.2)
Data from small imaging studies aiming to identify responders in patients treated with NAC suggest that response after two cycles of treatment is predictive of outcome. Although mpMRI has the advantage of better resolution of the bladder wall tissue planes as compared to CT, it is not ready yet for standard patient care. However, bladder mpMRI may be useful to inform on tumour stage after TURB and response to NAC [118]. So far PET/CT, MRI or DCE-MRI cannot accurately assess treatment response [293-296]. To identify progression during NAC, imaging is being used in many centres notwithstanding the lack of supporting evidence.
For responders to NAC, especially in those with a complete response (pT0 N0), treatment has a major positive impact on OS [297,298]. Therefore, reliable predictive markers to identify patients most likely to benefit from chemotherapy are needed. A recently reported study investigated how molecular subtypes impact pathological response and survival in patients receiving pre-operative cisplatin-based chemotherapy [299]. Patients with genomically unstable (GU) and urothelial-like (Uro) tumours had higher proportions of complete pathological response (16/31 [52%] and 17/54 [31%]), vs. five out of 24 (21%) for the basal/squamous (Ba/Sq) subtype following NAC and RC. Molecular subtype was independently associated with improved survival for patients with GU tumours (HR: 0.29, 95% CI: 0.11–0.79) and UroC tumours (HR: 0.37, 95% CI: 0.14–0.94) compared with Ba/Sq tumours, adjusting for clinical stage. Molecular tumour profiling might guide the use of NAC in the future but, as yet, this is not applicable in routine practice [300-302] (see Chapter 6 - Markers).
7.1.4. Role of neoadjuvant immunotherapy and chemo-immunotherapy
Inhibition of PD-1/PD-L1 checkpoint has demonstrated significant benefit in patients with unresectable and metastatic BC in the second-line setting and in platinum-ineligible PD-L1+ patients as first-line treatment using different agents. Checkpoint inhibitors are increasingly tested also in the neoadjuvant setting; either as monotherapy or in combination with chemotherapy or CTLA-4 checkpoint inhibition. Data from two phase II trials have been presented with encouraging results [240,241]. The results of the phase II trial using the PD-1 inhibitor pembrolizumab reported a complete pathological remission (pT0) in 42% and pathological response (< pT2) in 54% of patients, whereas in the single-arm phase II trial with atezolizumab a pathologic complete response rate of 31% was reported. In the recently published update to the ABACUS trial using single-agent atezolizumab, two-year DFS and OS were 68% (95% CI: 58–76) and 77% (95% CI: 68–85), respectively with two-year DFS in patients achieving a pathological complete response of 85% (95% CI: 65–94) [303].
Two recently published studies have investigated the use of neoadjuvant chemo-immunotherapy in patients with MIBC. In a phase II study of gemcitabine plus split-dose cisplatin and pembrolizumab in patients with MIBC, 22 of 39 patients (56% [95% CI: 40–72]) achieved < pT2N0 and 14 of 39 (36% [95% CI: 21–53]) achieved pT0N0 [304]. In a second phase II study evaluating neoadjuvant atezolizumab with gemcitabine and cisplatin; 27 of 39 patients (69%) were < pT2N0 and 16 (41%) pT0N0. No patient with < pT2N0 relapsed and four (11%) with > pT2N0 relapsed with a median follow-up of 16.5 months (range: 7.0–33.7 months) [305]. With the promising pathologic response rates, several larger studies are currently investigating the potential role for neoadjuvant chemo-immunotherapy in patients with MIBC.
At present, the results with immunotherapy alone, or in combination with chemotherapy, are promising but not yet approved in routine practice.
7.1.5. Summary of evidence and guidelines for neoadjuvant therapy
Summary of evidence | LE |
Neoadjuvant cisplatin-containing combination chemotherapy improves OS (5–8% at five years). | 1a |
Neoadjuvant treatment may have a major impact on OS in patients who achieve ypT0 or < ypT2. | 2a |
Currently immunotherapy with checkpoint inhibitors as monotherapy, or in different combinations with or without chemotherapy, is being tested in phase II and III trials. Initial results are promising. | - |
There are still no reliable tools available to select patients who have a higher probability of benefitting from NAC. In the future, genetic markers in a personalised medicine setting might facilitate the selection of patients for NAC and differentiate responders from non-responders. | - |
Recommendations | Strength rating |
If eligible for cisplatin-based chemotherapy, offer neoadjuvant cisplatin-based combination chemotherapy to patients with muscle-invasive bladder cancer (T2-T4a, cN0 M0). | Strong |
Do not offer NAC to patients who are ineligible for cisplatin-based combination chemotherapy. | Strong |
Only offer neoadjuvant immunotherapy to patients within a clinical trial setting. | Strong |
7.2. Pre- and post-operative radiotherapy in muscle-invasive bladder cancer
7.2.1. Post-operative radiotherapy
Given the high rates of local-regional failure after RC in patients with locally-advanced (pT3–4) BC, estimated at ~30%, as well as the high risk of distant failure and poor survival for these patients, there is an interest in adjuvant therapies that address both the risk of local and distant disease. Data on adjuvant RT after RC are limited and further prospective studies are needed, but a more recent phase II trial compared adjuvant sequential chemotherapy and radiation vs. adjuvant chemotherapy alone in 120 patients with locally-advanced disease and negative margins after RC (with one or more risk factors: > pT3b, grade 3, or node-positive), in a study population with 53% UC and 47% SCC. Addition of adjuvant RT to chemotherapy alone was associated with a statistically significant improvement in local relapse-free survival (at 2 years 96% vs. 69% favouring the addition of RT). Disease-free survival and OS also favoured the addition of RT, but those differences were not statistically significant and the study was not powered for those endpoints. Late-grade > 3 GI toxicity in the chemoradiation arm was low (7% of patients) [306].
A 2019 systematic review evaluating the efficacy of adjuvant radiation for BC or UTUC found no clear benefit of adjuvant radiation following radical surgery (e.g., cystectomy), although the combination of adjuvant radiation with chemotherapy may be beneficial in locally-advanced disease [307].
Adjuvant radiation might be considered in patients with pT3/pT4 pN0–2 urothelial BC following RC, although this approach has been evaluated in only a limited number of studies without conclusive data demonstrating improvements in OS. Radiation fields should encompass areas at risk for harbouring residual microscopic disease based on pathologic findings at surgery and may include the cystectomy bed and pelvic LNs. Doses in the range of 45 to 50.4 Gy may be considered. A small retrospective study of 25 patients (median age 64 years) evaluated acute and late toxicity of moderate doses of pelvic RT (range, 45–50.4 Gy). After a median follow-up of 10.4 months the authors concluded that orthotopic ileal neobladders can tolerate moderate radiation doses without significant induced morbidity. Most of the acute GI toxicity seen was grade 1, four patients developed acute grade 2 toxicity; three of whom had been treated by NAC [308].
For patients not treated with NAC, it may be reasonable to sandwich adjuvant radiation between cycles of adjuvant chemotherapy. The safety and efficacy of concurrent radiosensitising chemotherapy in the adjuvant setting needs further study.
7.2.2. Pre-operative radiotherapy
To date, six RCTs have been published investigating pre-operative RT, although all are from several decades ago. In the largest trial, pre-operative RT at a dose of 45 Gy was used, resulting in a significant increase in pathological complete response (9% to 34%) in favour of pre-operative RT, which was also a prognostic factor for survival [309]. The OS data were difficult to interpret since chemotherapy was used in a subset of patients only and more than 50% of patients (241/475) did not receive the planned treatment and were excluded from the final analyses. Two smaller studies using a dose of 20 Gy showed only a small survival advantage in > T3 tumours [310,311]. Two other small trials confirmed downstaging after pre-operative RT [312,313]. In a retrospective analysis of 1,846 evaluable patients, only 34 patients received RT prior to orthotopic neobladder reconstruction. The authors conclude that following pelvic RT, a neobladder is possible in highly selected patients with statistically similar peri-operative complication rates compared to patients who did not receive prior RT. Patient selection, with oncologic factors (positive urethral margins, nodal involvement, and extravascular disease) more commonly than technical factors (adhesions/difficult dissection, bleeding, urethral stricture) influencing conversion from a planned neobladder reconstruction [314].
A meta-analysis of five RCTs showed a difference in 5-year survival (OR: 0.71, 95% CI: 0.48–1.06) in favour of pre-operative RT [315]. However, the meta-analysis was potentially biased by data from the largest trial in which patients were not given the planned treatment. When the largest trial was excluded from the analysis, the OR became 0.94 (95% CI: 0.57–1.55), which was not significant.
A more recent RCT, comparing pre-operative vs. post-operative RT and RC (n = 100), showed comparable OS, DFS and complication rates [316]. Approximately half of these patients had UC, while the other half had SCC. In general, such older data is limited in being able to provide a robust evidence base for modern guideline recommendations.
7.2.3. Summary of evidence and guidelines for pre- and post-operative radiotherapy
Summary of evidence | LE |
No contemporary data exists to support that pre-operative RT for operable MIBC increases survival. | 2a |
Pre-operative RT for operable MIBC, using a dose of 45–50 Gy in fractions of 1.8–2 Gy, results in down-staging after 4 to 6 weeks. | 2 |
Limited evidence supports the safe use of pre- and post-operative RT in case a neobladder is planned or in situ. | 3 |
Limited high-quality evidence supports the use of pre-operative RT to decrease local recurrence of MIBC after RC. | 3 |
Addition of adjuvant RT to chemotherapy is associated with an improvement in local relapse-free survival following cystectomy for locally-advanced bladder cancer (pT3b–4, or node-positive). | 2a |
Recommendations | Strength rating |
Do not offer pre-operative radiotherapy (RT) for operable muscle-invasive bladder cancer since it will only result in down-staging, but will not improve survival. | Strong |
Do not offer pre-operative RT when subsequent radical cystectomy (RC) with urinary diversion is planned. | Strong |
Consider offering adjuvant RT in addition to chemotherapy following RC, based on pathologic risk (pT3b–4 or positive nodes or positive margins). | Weak |
7.3. Radical surgery and urinary diversion
7.3.1. Removal of the tumour-bearing bladder
7.3.1.1. Introduction
Standard treatment for patients with MIBC consists of RC, pelvic LN dissection, and urinary diversion, with- or without NAC [317]. An increasing focus on QoL contributes to a growing trend of utilizing bladder-sparing approaches, such as RT or chemoradiation in selected patients (see Section 7.5). Performance status and life expectancy influence the choice of primary management as well as the type of urinary diversion with RC being reserved for patients with a longer life expectancy without concomitant disease and a better PS. Frailty, nutritional status and decreased kidney function are conditions significantly related to an increased risk of post-operative adverse events (AEs) [318-320].
7.3.1.2. Radical cystectomy: timing
A meta-analysis including 19 studies concluded that a delay of > 3 months has a negative effect on OS (HR: 134, 95% CI: 1.18–1.53). Authors highlighted the lack of standardisation regarding the definition of delays which made it impossible to identify a clear cut-off time [321]. Overall conclusion was that BC patients scheduled for RC should be treated without delays to maximise survival.
7.3.2. Radical cystectomy: indications
Radical cystectomy is recommended in patients with T2–T4a, N0M0 disease, very high-risk NMIBC, BCG-refractory, BCG-relapsing and BCG-unresponsive NMIBC (see EAU Guidelines on Non-muscle-invasive Bladder Cancer [2]), as well as extensive papillary disease that cannot be controlled with TURBT and intravesical chemotherapy/immunotherapy alone.
Salvage cystectomy is indicated in non-responders to conservative therapy, i.e., recurrence after bladder-sparing treatment. It is also used as a purely palliative intervention, including for fistula formation, pain and recurrent uncontrollable haematuria (see Section 7.4.1 - Palliative cystectomy).
7.3.3. Radical cystectomy: technique and extent
Different approaches have been described to improve voiding and sexual function in patients undergoing RC for BC. No consensus exists regarding which approach preserves function best. Concern remains regarding the impact of ‘sparing-techniques’ on oncological outcomes.
7.3.3.1. Radical cystectomy in men
In men, standard RC includes removal of the bladder, prostate, seminal vesicles, distal ureters, and regional LNs.
7.3.3.1.1. Concomitant prostate cancer
A systematic review and meta-analysis of 13,140 patients showed an incidental prostate cancer rate of 24% [322]. Incidental prostate cancer was associated with higher age and lower 5-year OS. However, the lower OS can be explained by the higher age of patients with incidental prostate cancer. Pathological reporting of the specimens should follow the recommendations as presented in the EAU-EANM-ESTRO-ESUR-ISUP-SIOG Guidelines on Prostate Cancer [323].
7.3.3.1.2. Sexual-preserving techniques
Four main types have been described:
1. Prostate sparing cystectomy: part of or the whole prostate is preserved including seminal vesicles, vas deferens and neurovascular bundles.
2. Capsule sparing cystectomy: the capsule or peripheral part of the prostate is preserved with adenoma (including prostatic urethra) removed by TURP or en bloc with the bladder. Seminal vesicles, vas deferens and neurovascular bundles are also preserved.
3. Seminal sparing cystectomy: seminal vesicles, vas deferens and neurovascular bundles are preserved.
4. Nerve-sparing cystectomy: the neurovascular bundles are the only tissue left in place.
The systematic review on oncological and functional outcomes of sexual function-preserving cystectomy in men indentified 12 studies (n = 1,098) [324]. In the majority of cases, an open surgical approach was used and the urinary diversion of choice was an orthotopic neobladder. Median follow-up was longer than three years in nine studies, with three studies presenting results with a median follow-up longer than five years.
The majority of the studies included patients who were potent pre-operatively with organ-confined disease without tumour in the bladder neck and/or prostatic urethra. Prostate cancer was ruled out in all of the sexual-preserving cystectomy (SPC) techniques, except in the nerve-sparing approach [323].
Oncological outcomes did not differ between groups in any of the comparative studies that measured local recurrence, metastatic recurrence, DSS and OS, at a median follow-up of three to five years.
For techniques preserving prostatic tissue (prostate- or capsule-sparing), rates of incidental prostate cancer in the intervention group ranged from 0–15%. Incidental prostate cancer with ISUP grade > 4 was not reported.
Post-operative potency was significantly better in patients who underwent any type of SPC technique compared to conventional RC (p < 0.05), ranging from 80–90%, 50–100% and 29–78% for prostate-, capsule- or nerve-sparing techniques, respectively. Urinary continence, defined as the use of ‘no pads’ in the majority of studies, ranged from 88–100% (day-time continence) and from 31–96% (night-time continence) in the prostate-sparing cystectomy patients. No major differences were seen with regard to continence rates between any of these approaches.
The evidence base suggest that these procedures may yield better sexual outcomes than standard RC without compromising oncological outcomes. However, the overall quality of the evidence was moderate, and hence if a SPC technique is offered, patients must be carefully selected, counselled and closely monitored.
7.3.3.1.3. Summary of evidence and recommendations for sexual-preserving techniques in men
Summary of evidence | LE |
The majority of eligible patients motivated to preserve their sexual function will benefit from sexual-preserving techniques. | 2a |
None of the sexual-preserving techniques (prostate/capsule/seminal/nerve-sparing) have shown to be superior, and no particular technique can be recommended. | 3 |
Recommendations | Strength rating |
Only offer sexual-preserving techniques to eligible men very motivated to preserve their sexual function. | Strong |
Select patients based on: organ-confined disease; absence of any kind of tumour at the level of the prostate, prostatic urethra or bladder neck. | Strong |
7.3.3.2. Radical cystectomy in women
Historically, standard RC in women includes removal of the bladder, the entire urethra and adjacent vagina, uterus, distal ureters, and regional LNs. Pelvic floor disorders, sexual and voiding dysfunction in female patients are prevalent after RC [325]. As part of the pre-operative evaluation a gynaecological history should be obtained and patients should be counselled on the potential negative impact of RC on sexual function and/or vaginal prolapse. Most importantly, a history of cervical cancer screening, abnormal vaginal bleeding and a family history of breast and/or ovarian cancer should be recorded, as well as ruling out possible pelvic organ prolapse. Post-operatively, screening for sexual and urinary function and prolapse, is mandatory.
Pelvic organ-preserving techniques involve preserving the neurovascular bundle, vagina, uterus, ovaries or variations of any of the stated techniques. From an oncological point of view, concomitant malignancy in gynaecological organs is rare and local recurrences reported after RC are infrequent [326,327]. In premenopausal women, by preserving ovaries, hormonal homeostasis will be preserved, decreasing risk of cognitive impairment, cardiovascular diseases and loss of bone density. In case of an increased risk of hereditary breast or ovarian cancer (i.e., BRCA1/2 mutation carriers or patients with Lynch syndrome), salpingooophorectomy should be advised after childbearing and to all women over 40 years of age [328]. On the other hand, preservation of the uterus and vagina will provide the necessary support for the neobladder, thereby reducing the risk of urinary retention. It also helps to avoid post-operative prolapse as removal of the uterus predisposes to an anterior or posterior vaginal prolapse. In case of an already existing prolapse of the uterus, either isolated or combined with a vaginal prolapse, removing the uterus will be beneficial. It is noteworthy that by resecting the vaginal wall, the vagina shortens which could impair sexual satisfaction and function.
Based on retrospective low quality data only, a systematic review evaluating the advantages and disadvantages of sexual-function preserving RC and orthotopic neobladder in female patients concluded that in well-selected patients, sparing female reproductive organs during RC appears to be oncologically safe and provides improved functional outcomes [329]. Historically, patients selection has been limited to cT2 disease, but there are recent encouraging reports that support including women with more advanced T-stage and histological subtypes without compromising oncological outcomes [330].
Pelvic organ-preserving RC could be considered also in elderly and fragile patients as it may be beneficial from the point of reduced blood loss and quicker bowel recovery [331].
7.3.3.2.1. Summary of evidence and recommendations for sexual-preserving techniques in women
Summary of evidence | LE |
Data regarding pelvic organ-preserving RC for female patients remain immature. | 3 |
Recommendations | Strength rating |
Offer sexual organ-preserving techniques to eligible women to preserve their sexual function. | Strong |
Select patients based on: absence of tumour in the area to be preserved to avoid positive soft tissue margins; absence of pT4 urothelial carcinoma. | Strong |
7.3.4. Lymphadenectomy: role and extent
The optimal extent of lymphadectomy (LND) has not been established to date. Standard LND in MIBC patients involves removal of nodal tissue cranially up to the common iliac bifurcation, with the ureter being the medial border, and including the internal iliac, presacral, obturator fossa and external iliac nodes. The lateral borders are the genitofemoral nerves, caudally the circumflex iliac vein, the lacunar ligament and the LN of Cloquet [332]. Limited LND includes the nodes from the true pelvis, but excluding the deep obturator nodes. Extended LND includes the same boundaries as a standard LND, except for the cranial limit which is the region of the aortic bifurcation [333]. A super-extended LND extends cranially to the level of the inferior mesenteric artery [334].
Controversies in the clinical importance of LND are related to the question whether it should be considered a staging tool, a therapeutic procedure, or both.
7.3.4.1. Diagnostic value of lymphadenectomy
To understand the lymphatic spread in MIBC, two important autopsy studies have been performed. The first study analysed 367 patients with a history of cystectomy or MIBC at the time of autopsy. In total, 215 patients (59%) had node-positive disease [335]. In these patients 92% of the positive LNs were regional (perivesical or pelvic), 72% retroperitoneal and 35% abdominal.
The second autopsy study focused on the nodal yield when super-extended pelvic LND was performed. Substantial inter-individual differences were found with counts ranging from 10 to 53 nodes [336]. These findings demonstrate the limited utility of node count as a surrogate for extent of dissection, supporting a template-based LND instead.
In addition to autopsy studies, several authors adressed the spread of lymphatic disease by performing LN mapping studies in MIBC patients undergoing RC and (super)extended PLND [337-339]. These studies have demonstrated that LN-positive disease is present in approximately 25% of patients. In the group of node-positive patients, positive LNs cranial to the iliac bifurcation were present in over 40% of patients, however, skip LN metastasis were very rare (1%), as seen in autopsy studies. From a staging perspective only, these studies suggest that a standard LND should be sufficient to identify nearly all patients with node-positive disease.
7.3.4.2. Therapeutic value of lymphadenectomy
The therapeutic value of LND is a topic of continuous debate. To assess the oncological outcomes of different LND templates, a systematic review including 19 studies was performed [340].
Five studies compared LND vs. no LND and reported better oncological outcomes for the LND group. Seven out of twelve studies comparing (super)extended with limited or standard LND reported a beneficial outcome for (super)extended LND in at least a subset of patients. Two studies did not show a difference in outcome between extended and super-extended LND [340].
To date, the only prospective randomised data is available from the LEA trial performed in Germany. In this trial, patients with MIBC (n = 346) or T1G3 disease (n = 55) were included. Patients underwent either a limited LND (n= 203) or extended LND (n = 198). Survival differences between the groups were seen, in favour of extended LND. However, extended LND failed to show a significant advantage (the trial was designed to show an absolute improvement of 15% in 5-year RFS by extended LND) over limited LND for RFS, CSS, and OS.
In conclusion, there no high level data to support an extended LND, but data with lower level of evidence suggest that extended LND might be beneficial compared to more limited LND templates.
7.3.5. Robotic-assisted laparoscopic cystectomy
A number of recent systematic reviews comparing open RC (ORC) and robot-assisted RC (RARC) reach similar conclusions; RARC has an approximately one-day shorter length of hospital stay (LOS) and less blood loss, but a longer operative time. Complication rates seem similar for both approaches but all published reviews suffer from low quality data.
In minimally-invasive cystectomy, with increasing age, LOS is markedly shorter; up to 2.56 days in patients over 80 years old [341].
Although the low level of evidence of the studies included in these reviews remains a major limitation, a recent Cochrane review incorporating data from all five published RCTs corroborates most findings [342]. Time to recurrence, positive surgical margin rates, grade 3–5 complications and QoL were comparable for RARC and ORC, whilst transfusion rate was likely lower after RARC. For other endpoints outcomes were uncertain due to study limitations.
An economic evaluation (healthcare and societal perspective) of a Dutch prospective multi-centre comparative effectiveness study asessing ORC (n = 168) vs. RARC (n = 180) showed that both mean healthcare costs and societal costs per patient were significantly higher after RARC, resulting in an increase in QALYs of 0.02 [343].
Data on post-RC uretero-enteric stricture rates for both ORC and RARC remain inconclusive. Results are mainly reported by high-volume centres or derive from population-based studies with a large variety of endpoints and poor controlling of potential confounders, making comparison difficult [344-348]. Especially those managed by extracorporeal diversion (RARC-ECUD) tend to have more strictures compared to intracorporeal diversion (RARC-ICUD) [348]. This is explained by the need for more extensive dissection of ureter in RARC-ECUD, more tension, resulting in impaired blood supply [349,350].
Recurrence-free survival, CSS and OS have been documented as similar in all RCTs. A larger (n = 595) single-centre study with a median follow-up of over five years also found comparable recurrence and survival data, including atypical recurrences (defined as one or a combination of the following: portsite metastasis or peritoneal carcinomatosis) [351]. Interrestingly, Wei et al., detected residual cancer cells in pelvic washing specimens during or after, but not before, RARC in approximately half of the patients (9/17), which was associated with aggressive histological subtypes and cancer recurrence. These findings need confirmation in larger studies [352].
Most reviewed series offer extracorporeal reconstruction. Hussein et al., retrospectively compared extracorporeal reconstruction (n = 1,031) to intracorporeal reconstruction (n = 1,094); the latter was associated with a shorter operative time and fewer blood transfusions but more high-grade complications, which decreased over time [353]. A retrospective report from a high-volume centre found less (major) complications after intracorporeal reconstruction (n = 301) as compared to extracorporeal reconstruction (n = 375) and open RC (n = 272) [354].
A RCT comparing recovery and morbidity after ORC (n = 169) and RARC (n = 169) with intracorporeal diversion reported on the number of days alive and out of the hospital within 90 days of surgery which was 82 and 80 days, respectively [355]. In total, 89% of the patients underwent ileal conduit diversion. Thromboembolic complications and wound complications were less common with robotic surgery. Quality of life was initially worse after open surgery, but the difference was not significant after 12 weeks. There were no statistically significant differences in cancer recurrence or overall mortality at median follow-up of 18.4 months.
7.3.5.1. Summary of evidence and guidelines for robotic-assisted laparoscopic cystectomy
Summary of evidence | LE |
Robot-assisted radical cystectomy has longer operative time (1–1.5 hours) and higher costs, but shorter length of hospital stay (1–1.5 days) and less blood loss compared to ORC. | 1 |
Robotic cystectomy and open cystectomy may result in similar rates of (major) complications. | 2 |
Most endpoints, if reported, including intermediate-term oncological endpoint and QoL, are similar for RARC and ORC. | 2 |
Surgeons experience and institutional volume are considered the key factor for outcome of both RARC and ORC, not the technique. | 2 |
Recommendations | Strength rating |
Inform the patient of the advantages and disadvantages of open radical cystectomy (ORC) and robot-assisted radical cystectomy (RARC) to allow selection of the proper procedure. | Strong |
Select experienced centres, not specific techniques, both for RARC and ORC. | Strong |
7.3.6. Urinary diversion after radical cystectomy
Different types of segments of the intestinal tract can be used to reconstruct the urinary tract, including the ileum, colon and appendix, with ileum used in most cases. Several studies have compared advantages and disadvantages in terms of QoL, sexual function, urinary continence and body image between different urinary diversions [356], but further research evaluating the impact of tumour stage, functional- and socio-economic status are needed.
7.3.6.1. Different types of urinary diversion
For the choice of urinary diversion, comorbidity, cardiac, pulmonary and cognitive function are important factors that should be considered, along with the patient’s social support and preference (see Section patient selection/comorbidities). Age > 80 years is often considered to be the threshold after which neobladder reconstruction is not recommended. However, there is no exact age for a strict contraindication [357]. Randomised controlled trials comparing conduit diversion with neobladder or continent cutaneous diversion have not been performed.
7.3.6.1.1. Uretero-cutaneostomy
Ureteral diversion to the abdominal wall is the simplest form of cutaneous diversion. Operating time, complication rate, blood loss, transfusion rate, stay at intensive care and length of hospital stay are lower in patients treated with ureterocutaneostomy as compared to ileal conduit [358]. In frail patients and/or in those with a solitary kidney who need a supravesical diversion, uretero-cutaneostomy is the preferred procedure. In case patients have both kidneys and need a uretero-cutaneostomy, either one ureter, to which the other shorter one is attached end-to-side, is connected to the skin (trans-uretero-cutaneostomy) or both ureters may be directly anastomosed to the abdominal wall creating a stoma.
Due to the smaller diameter of the ureters, stoma stenosis and ascending UTIs have been observed more frequently for this technique as compared to using small or large bowel to create an intestinal stoma [359].
7.3.6.1.2. Ileal conduit
The ileal conduit is an established option with well-known/predictable results. Early complications (30-day cut off, used in most publications) include UTIs, pyelonephritis, ureteroileal leakage and stenosis which occur in 48% of patients [360].
7.3.6.1.3. Orthotopic neobladder
According to Dutch-, German- and Spanish bladder cancer registry data, an orthotopic bladder substitution to the urethra is used in approximately 10–20% of both male and female patients. Emptying of the reservoir anastomosed to the urethra requires abdominal straining, and sphincter relaxation. The terminal ileum is the GI segment most often used for orthotopic bladder substitution. Early and late morbidity in up to 22% of patients is reported [361].
Various forms of UUT reflux protection, including a simple isoperistaltic tunnel, ileal intussusception, tapered ileal prolongation implanted subserosally, and direct (sub)mucosal or subserosal ureteral implantation, have been described [362,363]. According to the long-term results, the UUT is protected sufficiently by either method [361].
A study comparing cancer control and patterns of disease recurrence in patients with neobladder and ileal conduit showed no difference in CSS between the two groups when adjusting for pathological stage [364]. Urethral recurrence in neobladder patients seems rare (0.8–13.7% [pooled estimate of 4.6% in both male and female patients, also considering the significantly higher recurrence rates in male patients]) [365]. These results indicate that neobladder in male and female patients does not compromise the oncological outcome of cystectomy.
7.3.6.1.4. Continent cutaneous urinary diversion
Continent cutaneous urinary diversion (a low-pressure detubularised ileal reservoir for self-catheterisation) and uretero-rectosigmoidostomy are rarely used techniques nowadays, due to their high complication rates, including stomal stenosis, incontinence in the continent cutaneous diversion, UUT infections and stone formation in case of uretero-rectosigmoidostomy [366].
7.3.6.2. Patient selection
Ensuring that patients make a well-informed decision about the type of urinary diversion is associated with less decision regret post-operatively, independent of the method selected [367]. Therefore, all applicable forms of urinary diversion should be discussed, taking into account patient preference, comorbidities, age and tumour characteristics.
Diagnosis of an invasive urethral tumour prior to cystectomy leads to urethrectomy which is a contraindication for a neobladder reconstruction. Non-muscle-invasive BC in prostatic urethra or bladder neck biopsies does not necessarily preclude orthotopic neobladder substitution, provided that patients undergo regular follow-up cystoscopy and urinary cytology [368]. In women undergoing RC the rate of concomitant urethral malignancy has been reported to range from 12–16% [369]. Localisation of the primary tumour at the bladder neck correlated strongly with concomitant urethral malignancy. Bladder neck biopsies prior to RC are important in women scheduled for an orthotopic bladder substitute [370].
In the presence of positive LNs, orthotopic neobladder can be considered in case of N1 disease, but not in N2 or N3 tumours [371].
Oncological results after orthotopic neobladder or illial conduit are similar in terms of local or distant metastasis recurrence, but secondary urethral tumours seem less common in patients with a neobladder compared to those with conduits or continent cutaneous diversions [372].
Patients undergoing continent urinary diversion must be motivated to learn about their diversion and to be manually skilful to be able to deal with their diversion. Contraindications to continent urinary diversions include:
- debilitating neurological and psychiatric illnesses;
- limited life expectancy;
- severe impaired liver or renal function.
Relative contraindications for an orthotopic neobladder are high-dose pre-operative RT, complex urethral strictures and severe urethral sphincter-related incontinence [373].
A retrospective study including 1,383 patients showed that the risk of a decline in estimated glomerular filtration rate (eGFR) did not significantly differ after ileal conduit vs. neobladder in patients with pre-operative chronic kidney disease 2 (eGFR 60–89 mL/min/1.73 m2) or 3a (eGFR 45–59 mL/min/1.73 m2) [374]. Only age and anastomotic strictures were found to be associated with a decline in eGFR.
Currently, it is not possible to recommend a particular type of urinary diversion. However, most institutions prefer ileal orthotopic neobladders and ileal conduits based on clinical experience. In selected patients, such as patients with a single kidney, uretero-cutaneostomy is surgically the least burdensome type of diversion. Recommendations related to RC and urinary diversions are listed in Section 7.3.10.
7.3.6.3. Peri-operative care
Patients treated according to a ‘Fast tract’/ERAS (Early Recovery After Surgery) protocol have shown to score better on the emotional and physical functioning scores and suffer less from wound healing disorders, fever and thrombosis [375].
Pre-operatively, the ERAS protocol recommends no bowel prepation or fasting. Other components are, for example, same day admission, as well as carbohydrate loading and a pre-operative exercise programme.
Important post-operative components of the ERAS protocol are pain management, which involves reducing the use of opioids; increasing the use of high-dose acetaminophen and/or ketorolacs (only as breakthrough pain medication) and patients on ERAS experience more pain as compared to patients on a traditional protocol (Visual Analogue Scale [VAS] 3.1 vs. 1.1, p < 0.001), but post-operative ileus decreased from 22% to 7.3%
(p = 0.003) [376].
Venous thromboembolism (VTE) prophylaxis may be implemented as part of an ERAS protocol. A single-centre non-randomised study showed a significant lower 30-day VTE incidence rate in patients treated for 28 days with enoxaparin compared to patients without prophylaxis [377]. Data from the Ontario Cancer Registry including 4,205 cystectomy patients of whom 1,084 received NAC showed that VTE rates are higher in patients treated with NAC as compared to patients treated with cystectomy only (12% vs. 8%, p = 0.002) [378].
7.3.7. Morbidity and mortality
In four retrospective studies and one population-based cohort study, the peri-operative mortality after RC was reported as 2.1–3.2% at 30 days and 3.4–8.0% at 90 days [379,380]. Morbidity rates differ strongly according to the reporting system used. Using the Clavien-Dindo Classification system complication rates ranged from 50–88% (I–IV) and severe complications from 30–42% (> III) [381-384]. In large national databases and institutional series, readmission rates are approximately 25% within 30 days of discharge [385]. Late morbidity was usually linked to the type of urinary diversion (see also above). Early morbidity associated with RC for NMIBC (at high risk for disease progression) is similar and no less than that associated with muscle-invasive tumours [386,387]. In general, lower morbidity and (peri-operative) mortality have been observed by surgeons and in hospitals with a higher case load and therefore more experience [388-391].
Table 7.1: Management of neobladder morbidity (30-64%)
CLAVIEN System | Morbidity | Management | |
Grade I | Any deviation from the normal post-operative course without the need for pharmacological treatment or surgical, endoscopic and radiological interventions. Allowed therapeutic regimens are: drugs such as antiemetics, antipyretics, analgesics, diuretics and electrolytes and physiotherapy. This grade also includes wound infections opened at the bedside. | Immediate complications: | |
Post-operative ileus | Nasogastric intubation (usually removed at day 1) Chewing gum Avoid fluid excess and hypovolemia (provoke splanchnic hypoperfusion) | ||
Post-operative nausea and vomiting | Antiemetic agent Nasogastric intubation | ||
Urinary infection | Antibiotics, no ureteral catheter removal Check the 3 drainages (ureters and neobladdder) | ||
Ureteral catheter obstruction | Inject 5 cc saline in the ureteral catheter to resolve the obstruction Increase volume infusion to increase diuresis | ||
Intra-abdominal urine leakage (anastomosis leakage) | Check and reposition drainages, if needed | ||
Anaemia well tolerated | Martial treatment | ||
Late complications: | |||
Non compressive lymphocele | Watchful waiting | ||
Mucus cork | Catheterise and rinse the bladder | ||
Incontinence | Urine analysis (infection), echography (post-void residual) Physiotherapy | ||
Retention | Drainage and self-catheterisation education | ||
Ureteral reflux | No treatment if asymptomatic | ||
Grade II | Requiring pharmacological treatment with drugs other than those allowed for grade I complications. Blood transfusions and total parenteral nutrition are also included. | Anaemia badly tolerated or if myocardial cardiopathy history | Transfusion1 |
Pulmonary embolism | Heparinotherapy2 | ||
Pyelonephritis | Antibiotics and check kidney drainage (nephrostomy if necessary) | ||
Confusion or neurological disorder | Neuroleptics and avoid opioids | ||
Grade III | Requiring surgical, endoscopic or radiological intervention | Ureteral catheter accidentally dislodged | Reposition the ureteral catheter |
Anastomosis stenosis (7%) | Renal drainage (ureteral catheter or nephrostomy) | ||
III-a | Intervention not under general anaesthesia | Compressive lymphocele | Transcutaneous drainage |
III-b | Intervention under general anaesthesia | Ileal anastomosis leakage | Ileostomy, as soon as possible |
Evisceration | Surgery in emergency | ||
Compressive lymphocele | Surgery (marsupialisation) | ||
Grade IV | Life-threatening complication (including central nervous system complications: brain haemorrhage, ischaemic stroke, subarachnoid bleeding, but excluding transient ischaemic attacks) requiring intensive care/ intensive care unit management. | Neobladder rupture | Nephrostomy and indwelling catheter/surgery for draining the neobladder |
Severe sepsis | Antibiotics and check all the urinary drainages and CT scan in emergency | ||
IV-a | Single organ dysfunction | Non-obstructive renal failure | Bicarbonate/aetiology treatment (including dialysis) |
IV-b | Multi-organ dysfunction | Obstructive pyelonephritis and septicaemia | Treatment at intensive care unit, including urinary drainage and antibiotics |
Grade V | Death of a patient | ||
Suffix ‘d’ | If the patient suffers from a complication at the time of discharge, the suffix “d” (for ‘disability’) is added to the respective grade of complication. This label indicates the need for a follow-up to fully evaluate the complication. | ||
1 A systematic review showed that peri-operative blood transfusion (PBT) in patients who undergo RC correlates with increased overall mortality, CSM and cancer recurrence. The authors hypothesised that this may be caused by the suggested immunosuppressive effect of PBT. In a retrospective study, Buchner and co-workers showed 5-year decreased CSS in cases where intra-operative blood transfusion (CSS decreased from 67% to 48%) or post-operative blood transfusion (CSS decreased from 63% to 48%) were given 393.
2 Hammond and co-workers reviewed 20,762 cases of VTE after major surgery and found cystectomy patients to have the second-highest rate of VTE among all cancers studied 394. These patients benefit from 30 days low-molecular-weight heparin prophylaxis. Subsequently, it was demonstrated that BMI > 30 and non-urothelial BCs are independently associated with VTE after cystectomy. In these patients extended (90 days) heparin prophylaxis should be considered 378.
7.3.8. Survival
Of all cancers, bladder cancer ranks 13th in terms of mortality, with rates decreasing particularly in the most developed countries [395].
Disease-free survival and OS in a large population-based study was 35% and 58% at ten years, respectively [396]. However, the 5-year OS in node-positive patients who underwent cystectomy was 18% [397].
A systematic review including 57 studies (n = 30,293) assessed the long-term survical of patients treated with trimodality therapy (TMT) and RC [396]. Ten-year OS was 30.9% and 35.1%, for TMT and RC, respectively with a mean DSS of 50.9% for TMT and 57.8% for RC. For T2 disease, 10-year DSS was 69% and 78.9% for TMT and RC, respectively and for T3/T4 disease 43.5% and 43.1% for TMT and RC, respectively. Three percent of the patients (812 of 27,867) received NAC, resulting in 5-year OS and DSS in downstaged patients (< pT1) at RC of 75.7% and 88.3%, respectively.
7.3.9. Impact of hospital and surgeon volume on treatment outcomes
In a systematic review including 40 retrospective studies with 56,000 patients, the impact of hospital and/or surgeon volume and peri-operative outcomes of RC was assessed [398]. A higher hospital volume was associated with lower in-hospital, 30-day and 90-day mortality. In addition, higher volume hospitals were more likely to have lower positive surgical margins, higher number of LNDs and neobladders and lower complication rates. For surgeon volume, less evidence was available. This study suggested performing at least 10 RCs per centre annually and preferably more than 20. Recently, a nationwide analysis of the Dutch Cancer Registry including almost 9,500 patients between 2008 and 2018 reported decreased 30- and 90-day mortality rates for annual hospital volumes of > 30 RCs. Furthermore, this study showed no true plateau curve for 30- and 90-day mortality beyond 30 RCs supporting the ‘more is better’ principle [399,400].
7.3.10. Summary of evidence and guidelines for radical cystectomy and urinary diversion
Summary of evidence | LE |
Higher RC hospital volume is associated with lower post-operative mortality rates and higher quality of care. | 3 |
Radical cystectomy includes removal of regional LNs. | 3 |
There are data to support that extended vs. standard LND improves survival after RC. | 3 |
No conclusive evidence exists as to the optimal extent of LND. | 2a |
Ensuring that patients are well informed about the various urinary diversion options prior to making a decision may help prevent or reduce decision regret, independent of the method of diversion selected. | 3 |
The type of urinary diversion does not affect oncological outcome. | 3 |
The use of extended VTE prophylaxis significantly decreases the incidence of VTE after RC. | 3 |
In patients aged > 80 years with MIBC, cystectomy is an option. | 3 |
Surgical complications of cystectomy and urinary diversion should be reported using a uniform grading system. Currently, the best-adapted grading system for cystectomy is the Clavien Dindo grading system. | 2b |
Recommendations | Strength rating |
Do not delay radical cystectomy (RC) for > 3 months as it increases the risk of progression and cancer-specific mortality, unless the patient receives neoadjuvant chemotherapy. | Strong |
Perform at least 10, and preferably > 20, RCs per hospital/per year. | Strong |
Before RC, fully inform the patient about the benefits and potential risks of all possible alternatives. The final decision should be based on a balanced discussion between the patient and the surgeon. | Strong |
Do not offer an orthotopic bladder substitute diversion to patients who have an invasive tumour in the urethra or at the level of urethral dissection. | Strong |
Do not offer pre-operative bowel preparation. | Strong |
Employ ‘Fast track’ measurements to reduce the time to bowel recovery. | Strong |
Offer pharmacological VTE prophylaxis, such as low-molecular-weight heparin to RC patients, starting the first day post-surgery, for a period of at least 4 weeks. | Strong |
Offer RC to patients with T2–T4a, N0M0 disease or very high-risk non-muscle-invasive bladder cancer. | Strong |
Perform a lymph node dissection as an integral part of RC. | Strong |
Figure 7.1: Flow chart for the management of T2–T4a N0M0 urothelial bladder cancer

7.4. Palliative and salvage cystectomy
Unresectable locally-advanced tumours (T4b, invading the pelvic or abdominal wall) may be accompanied by debilitating symptoms, including bleeding, pain, dysuria and urinary obstruction. These patients are candidates for palliative treatments, such as palliative RT. If control of the symptoms is not possible by less invasive methods, patients may be offered a palliative cystectomy with urinary diversion or urinary diversion only. Palliative cystectomy carries the greatest morbidity, particularly in patients with a poor PS. In a series of 74 patients who underwent palliative cystectomy, severe complications (Clavien-Dindo grade > 3) occurred in 30%. The 30-day mortality rate was 9% and at eight months follow-up, 70% had died [401].
In a retrospective single-centre analysis, Pieretti et al., grouped 265 patients into salvage cystectomy post-TMT, primary cystectomy or primary cystectomy with prior history of non-TMT abdominal or pelvic RT. Post-TMT salvage cystectomy was associated with a higher incidence of any late (HR: 2.3, p = 0.02) and major late complications (HR: 2.1, p < 0.05) but there was no difference in DSS (p = 0.8) or OS (p = 0.9) between the groups [402].
7.4.1. Guidelines for palliative and salvage cystectomy
Recommendations | Strength rating |
Offer radical cystectomy as a palliative treatment to patients with locally-advanced tumours (T4b). | Weak |
Offer palliative cystectomy to patients with symptoms if control is not possible by less invasive methods. | Weak |
7.4.1.1. EAU-ESMO consensus statements on the management of advanced- and variant bladder cancer [9,10]*
Consensus statement |
In patients with clinical T4 or clinical N+ disease (regional), radical chemoradiation can be offered accepting that this may be palliative rather than curative in outcome. |
Chemoradiation should be given to improve local control in cases of inoperable locally-advanced tumours. |
*Only statements which met the a priori consensus threshold across all three stakeholder groups are listed(defined as > 70% agreement and < 15% disagreement, or vice versa).
7.4.2. Supportive care
7.4.2.1. Obstruction of the upper urinary tract
Unilateral (best kidney) or bilateral nephrostomy tubes provide the easiest solution for UUT obstruction, but patients find the tubes inconvenient and prefer ureteral stenting. However, stenting can be difficult to achieve. Stents must be regularly replaced and there is the risk of stent obstruction or displacement. Another possible solution is a urinary diversion with, or without, a palliative cystectomy.
7.4.2.2. Bleeding and pain
In the case of bleeding, the patient must be screened first for coagulation disorders or the patient’s use of anticoagulant drugs must be reviewed. Transurethral (laser) coagulation may be difficult in a bladder full of tumour or with a bleeding tumour. Intravesical rinsing of the bladder with 1% silver nitrate or 1–2% alum can be effective [403]. This can usually be done without any anaesthesia. The instillation of formalin (2.5–4% for 30 minutes) is a more aggressive and painful procedure, requiring anaesthesia. Formalin instillation has a higher risk of side-effects, e.g., bladder fibrosis, but is more likely to control the bleeding [403]. Vesicoureteral reflux should be excluded to prevent renal complications.
Radiation therapy is another common strategy to control bleeding and is also used to control pain. An older study reported control of haematuria in 59% of patients and pain control in 73% [404]. Irritative bladder and bowel complaints due to irradiation are possible, but are usually mild. Non-conservative options are embolisation of specific arteries in the small pelvis, with success rates as high as 90% [403]. Radical surgery is a last resort and includes cystectomy and diversion (see above, Section 7.4.1).
7.5. Bladder-sparing treatments for localised disease
7.5.1. Transurethral resection of bladder tumour
Transurethral resection of bladder tumour alone in MIBC patients is only possible as a therapeutic option if tumour growth is limited to the superficial muscle layer and if re-staging biopsies are negative for residual (invasive) tumour [405]. In general, approximately 50% of patients will still have to undergo RC for recurrent MIBC with a disease-specific mortality rate of up to 47% in this group [406]. A disease-free status at re-staging TURB appears to be crucial in making the decision not to perform RC [407,408]. A prospective study by Solsona et al., including 133 patients after radical TURB and re-staging negative biopsies, reported a 15-year follow-up [408]. Thirty per cent of patients had recurrent NMIBC and went on to intravesical therapy, and 30% (n = 40) progressed, of which 27 died of BC. After five, ten, and fifteen years, the results showed CSS rates of 81.9%, 79.5%, and 76.7%, respectively and PFS rates with an intact bladder of 75.5%, 64.9%, and 57.8%, respectively.
In conclusion, TURB alone should only be considered as a therapeutic option for muscle-invasive disease after radical TURB, when the patient is unfit for cystectomy, or refuses open surgery, or as part of a TMT bladder-preserving approach.
7.5.1.1. Guideline for transurethral resection of bladder tumour
Recommendation | Strength rating |
Do not offer transurethral resection of bladder tumour alone as a curative treatment option as most patients will not benefit. | Strong |
7.5.2. External beam radiotherapy
Current RT techniques with soft-tissue matching and image guidance result in superior bladder coverage and a reduced integral dose to the surrounding tissues. The target total dose (to bladder and/or bladder tumour) for curative EBRT in BC is 64–66 Gy [409,410]. A reasonable alternative is moderately hypofractionated EBRT to 55 Gy in 20 fractions which has been suggested to be non-inferior to 64 Gy in 32 fractions in terms of invasive locoregional control, OS, and late toxicity. In a phase II study, 55 patients (median age 86) with BC, unfit for cystectomy or even daily RT, were treated with 6-weekly doses of 6 Gy [411]. Forty-eight patients completed EBRT with acceptable toxicity and 17% showed local progression after two years demonstrating good local control with this more ultra-hypofractionated schedule.
Elective treatment to the LNs is optional and should take into account patient comorbidities and the risks of toxicity to adjacent critical structures. For node-positive disease, consider boosting grossly involved nodes to the highest achievable dose that does not violate normal tissue constraints based on the clinical scenario.
The use of modern standard EBRT techniques results in major related late morbidity of the urinary bladder or bowel in less than 5% of patients [412]. Acute diarrhoea is reduced even more with intensity-modulated RT [413]. Important prognostic factors for outcome include response to EBRT, tumour size, hydronephrosis, presence of CIS, and completeness of the initial TURB. Additional prognostic factors reported are age and stage [414].
With the use of modern EBRT techniques, efficacy and safety results seem to have improved over time. A 2002 Cochrane analysis demonstrated that RC has an OS benefit compared to RT [415], although this was not the case in a 2014 retrospective review using a propensity score analysis [416].
In a 2017 retrospective cohort study of U.S. National Cancer Database data, patients over 80 were identified with cT2–4, N0–3, M0 BC, who were treated with curative EBRT (60–70 Gy, n = 739) or concurrent chemoradiotherapy (n = 630) between 2004 and 2013 [417]. The 2-year OS was 42% for EBRT vs. 56% for chemoradiotherapy (p < 0.001). For EBRT a higher RT dose and a low stage were associated with improved OS.
In conclusion, although EBRT results seem to improve over time, EBRT alone does not seem to be as effective as surgery or TMT therapy (see Section 7.5.4). Factors that influence outcome should be considered. However, EBRT can be an alternative treatment in patients unfit for radical surgery or concurrent chemotherapy, and it can also be effective in helping control bleeding.
7.5.2.1. Summary of evidence and guideline for external beam radiotherapy
Summary of evidence | LE |
External beam RT alone should only be considered as a therapeutic option when the patient is unfit for cystectomy. | 3 |
Radiotherapy can also be used to stop bleeding from the tumour when local control cannot be achieved by transurethral manipulation. | 3 |
Recommendation | Strength rating |
Do not offer radiotherapy alone as primary therapy for localised bladder cancer. | Strong |
7.5.2.2. EAU-ESMO consensus statements on the management of advanced- and variant bladder cancer [9,10]*
Consensus statement |
Radiotherapy alone (single block) is not the preferred radiotherapeutic schedule. |
Radiotherapy for bladder preservation should be performed with IMRT and IGRT to reduce side effects. |
Dose escalation above standard radical doses to the primary site in case of bladder preservation, either by IMRT or brachytherapy, is not recommended. |
*Only statements which met the a priori consensus threshold across all three stakeholder groups are listed(defined as > 70% agreement and < 15% disagreement, or vice versa).IGRT = image-guided radiotherapy; IMRT = intensity-modulated radiotherapy.
7.5.3. Chemotherapy
Chemotherapy alone rarely produces durable complete remissions. In general, a clinical complete response rate of up to 56% is reported in some series, which must be weighed against a staging error of > 60% [469,470]. Response to chemotherapy is a prognostic factor for treatment outcome and eventual survival although it may be confounded by patient selection [418].
Several groups have reported the effect of chemotherapy on resectable tumours (neoadjuvant approach), as well as unresectable primary tumours [259,276,419,420]. Neoadjuvant chemotherapy with two to three cycles of MVAC or CMV has led to a down-staging of the primary tumour in various prospective series [259,276,419].
A bladder-conserving strategy with TURB and systemic cisplatin-based chemotherapy has been reported several years ago and could lead to long-term survival with intact bladder in a highly selected patient population [421].
A recent large retrospective analysis of a U.S. National Cancer Database cohort reported on 1,538 patients treated with TURB and multi-agent chemotherapy [422]. The two and 5-year OS for all patients was 49% and 32.9% and for cT2 patients it was 52.6% and 36.2%, respectively. While these data show that long-term survival with intact bladder can be achieved in a subset of patients it is not recommended for routine use.
7.5.3.1. Summary of evidence and guideline for chemotherapy
Summary of evidence | LE |
Complete and partial local responses have been reported with cisplatin-based chemotherapy as primary therapy for locally-advanced tumours in highly selected patients. | 2b |
Recommendation | Strength rating |
Do not offer chemotherapy alone as primary therapy for localised bladder cancer. | Strong |
7.5.4. Trimodality bladder-preserving treatment
Bladder preservation as an alternative to RC is generally reserved for patients with smaller solitary tumours, negative nodes, no extensive or multifocal CIS, no tumour-related hydronephrosis, and good pre-treatment bladder function. Trimodality bladder-preserving treatment should also be considered in all patients with a contraindication for surgery, either a relative or absolute contraindication since the factors that determine fitness for surgery and chemoradiotherapy differ.
Trimodality therapy combines TURB, chemotherapy and RT. The rationale to combine TURB with RT is to achieve maximal local tumour control in the bladder and adjacent nodes. The addition of radiosensitising chemotherapy or other radiosensitisers (mentioned below) is aimed at the potentiation of RT. Micrometastases are targeted by platinum-based combination chemotherapy (for details see Section 7.1). The aim of TMT is to preserve the bladder and QoL without compromising oncological outcome. There are no definitive contemporary data supporting the benefit of using neoadjuvant or adjuvant chemotherapy combined with chemoradiation. Patient selection is critical in achieving good outcomes [423]. Whether a node dissection should be performed before TMT as in RC remains unclear [9,10].
There are no successfully completed RCTs comparing the outcome of TMT with RC, but TMT using chemoradiation has been shown to be superior to RT alone [424-426]. Many of the reported series have differing characteristics as compared to the larger surgical series, which typically have median ages in the mid-to-late 60s compared to mid-70s for some large RT series (reviewed by James, et al. [424]).
In the case of TMT, two distinct patterns of care emerge; treatment aimed at patients fit for cystectomy who elect TMT or refuse cystectomy, and treatment aimed at older, less fit, patients. For the former category, TMT presents selective bladder preservation and in this case the initial step is a radical TURB where as much tumour as possible should be resected. In this case appropriate patient selection (e.g., T2 tumours, no CIS) is crucial [427,428]. Even in case of an initial presumed complete resection, a second TUR has been suggested to reveal tumour in > 50% of patients and subsequently improves 5-year OS in case of TMT [429]. For patients who are not candidates for cystectomy, less stringent criteria can be applied, but extensive CIS and poor bladder function should both be regarded as relative contraindications.
A collaborative review has described the principles of TMT [423]. For radiation, two schedules are most commonly used; historically within the RTOG a split-course format with interval cystoscopy [425] and single-phase treatment which is now more commonly used [424]. A conventional radiation schedule includes EBRT to the bladder and limited pelvic LNs with an initial dose of 40-45 Gy, with a boost to the whole bladder of 50–54 Gy and a further tumour boost to a total dose of 60–66 Gy. If not boosting the tumour, it is also reasonable for the whole bladder to be treated to 59.4–66 Gy. For node-positive disease, consider boosting grossly involved nodes to the highest achievable dose that does not violate normal tissue constraints. Therefore, elective treatment to the LNs (when node negative) is optional and should take into account patient comorbidities and the risks of toxicity to adjacent critical structures.
A reasonable radiation dosing alternative to conventional fractionation when treating the bladder-only fields is moderately hypofractionated EBRT to 55 Gy in 20 fractions which has been suggested to be non-inferior to 64 Gy in 32 fractions in terms of invasive loco-regional control, OS and late toxicity [409,430].
Different chemotherapy regimens have been used, but most evidence exists for cisplatin [431] and mitomycin-C plus 5-FU [424]. In addition to these agents, other regimens have also been used such as gemcitabine and hypoxic cell sensitisation with nicotinamide and carbogen, without clear preference for a specific radiosensitiser [9,10]. In a recently published phase II RCT, twice-a-day radiation plus 5-FU/cisplatin was compared to once-daily radiation plus gemcitabine [432]. Both arms were found to result in a > 75% free from distant metastases at 3 years (78% and 84%, respectively). Therefore, there are options for non-cisplatin candidates such as 5-FU/mitomycin-C or low-dose gemcitabine.
Five-year CSS and OS rates vary between 50%–84% and 36%–74%, respectively, with salvage cystectomy rates of 10–30% [423,424,427,431,433]. The Boston group reported on their experience in 66 patients with mixed histological subtypes treated with TMT and found similar complete response, OS, DSS and salvage cystectomy rates as in UC [434]. The majority of recurrences post-TMT are non-invasive and can be managed conservatively [424]. In contemporary series, salvage cystectomy is required in about 10–15% of patients treated with TMT and can be curative [424,427,433]. Current data suggest that major late complication rates are slightly higher but remain acceptable for salvage- vs. primary cystectomy [435].
A meta-analysis of individual patient data from the BC2001 and BCON studies recently reported 10-year follow-up results [409]. The authors conclude that moderately hypofractionated RT with 55 Gy in
20 fractions over 4 weeks should be the new standard of care for bladder-preserving management of MIBC. The meta-analysis did not show a significant difference in late toxicity between fractionation regimens used and no difference was observed in patient-reported HRQoL in the long term after recovery from acute toxicity in the BC2001 trial. Published 5-year patient-reported outcomes showed excellent preservation of daily function with both fractionation schedules throughout the follow-up period.
A sub-analysis of two RTOG trials looked at complete response (T0) and near-complete response (Ta or Tis) after TMT [436]. After a median follow-up of 5.9 years 41/119 (35%) of patients experienced a bladder recurrence, and fourteen required salvage cystectomy. There was no difference between complete and near-complete responders. Non-muscle-invasive BC recurrences after complete response to TMT were reported in 25% of patients by the Boston group, sometimes over a decade after initial treatment [437]. A NMIBC recurrence was associated with a lower DSS, although in properly selected patients, intravesical BCG could avoid immediate salvage cystectomy.
The differential impact of RC vs. TMT on long-term OS is lacking a randomised comparison and rigorous prospective data. A propensity score matched institutional analysis has suggested similar DSS and OS between TMT and RC [433]. Two retrospective analyses of the U.S. National Cancer Database from 2004–2013 with propensity score matching compared RC to TMT. Ritch et al., identified 6,606 RC and 1,773 TMT patients [438]. Worse survival was linked to higher age, comorbidity and tumour stage. After modelling, TMT resulted in a lower mortality at one year (HR: 0.84, 95% CI: 0.74–0.96, p = 0.01). However, in years 2 and onwards, there was a significant and persistent higher mortality after TMT (year 2: HR: 1.4, 95% CI: 1.2–1.6, p < 0.001; and year 3 onwards: HR: 1.5, 95% CI: 1.2–1.8, p < 0.001). The second analysis was based on a larger cohort, with 22,680 patients undergoing RC; 2,540 patients received definitive EBRT and 1,489 TMT [439]. Survival after modelling was significantly better for RC compared to any EBRT, definitive EBRT and TMT (HR: 1.4, 95% CI: 1.2–1.6) at any time point. In general, such population-based studies are limited by confounding, misclassification, and selection bias. A systematic review including 57 studies and over 30,000 patients comparing RC and TMT found improved 10-year OS and DSS for TMT, but for the entire cohort OS and DSS did not significantly differ between RC and TMT [396]. Complete response after TMT resulted in significantly better survival, as did down-staging after TURB or NAC in case of RC.
Overall significant late pelvic (GI/genitourinary [GU]) toxicity rates after TMT are low and QoL is good [424,440,441]. A combined analysis of survivors from four RTOG trials with a median follow-up of 5.4 years showed that combined-modality therapy was associated with low rates of late grade 3 toxicity (5.7% GU and 1.9% GI). No late grade 4 toxicities or treatment-related deaths were recorded [440]. A retrospective study showed QoL to be good after TMT and in most domains better than after cystectomy, although prospective validations are needed [442]. One option to reduce side effects after TMT is the use of IMRT and image-guided RT
(IGRT) [9,10,443].
A bladder-preserving TMT strategy requires very close multidisciplinary cooperation [9,10]. This was also highlighted by a Canadian group [444]. In Ontario between 1994 and 2008 only 10% (370/3,759) of patients with cystectomy had a pre-operative radiation oncology consultation, with high geographical variations. Independent factors associated with this consultation included advanced age (p < 0.001), greater comorbidity (p < 0.001) and earlier year of diagnosis (p < 0.001). A bladder-preserving TMT strategy also requires a high level of patient compliance. Even if a patient has shown a clinical response to a TMT bladder-preserving strategy, the bladder remains a potential source of recurrence, hence long-term life-long bladder monitoring is essential and patients should be counselled that this will be required.
7.5.4.1. Summary of evidence and guidelines for trimodality bladder-preserving treatment
Summary of evidence | LE |
In a selected patient population, long-term survival rates of TMT bladder-preserving treatment are comparable to those of early cystectomy. | 2b |
Recommendations | Strength rating |
Offer surgical intervention or trimodality bladder-preserving treatments (TMT) to appropriate candidates as primary curative therapeutic approaches since they are more effective than radiotherapy alone. | Strong |
Offer TMT as an alternative to selected, well-informed and compliant patients, especially for whom radical cystectomy is not an option or not acceptable. | Strong |
7.5.4.2. EAU-ESMO consensus statements on the management of advanced- and variant bladder cancer [9,10]*
Consensus statement |
Candidates for curative treatment, such as cystectomy or bladder preservation, should be clinically assessed by at least an oncologist, a urologist, a radiation oncologist (in case adjuvant radiotherapy or bladder preservation is considered) and a neutral HCP such as a specialist nurse. |
An important determinant for patient eligibility in case of bladder-preserving treatment is absence of carcinoma in situ. |
An important determinant for patient eligibility in case of bladder-preserving treatment is absence or presence of hydronephrosis. |
When assessing patient eligibility for bladder preservation, the likelihood of successful debulking surgery should be taken into consideration (optimal debulking). |
In case of bladder preservation with radiotherapy, combination with a radiosensitiser is always recommended to improve clinical outcomes, such as cisplatin, 5-FU/MMC, carbogen/nicotinamide or gemcitabine. |
Radiotherapy for bladder preservation should be performed with IMRT and IGRT to reduce side effects. |
Dose escalation above standard radical doses to the primary site in case of bladder preservation, either by IMRT or by brachytherapy, is not recommended. |
*Only statements which met the a priori consensus threshold across all three stakeholder groups are listed(defined as > 70% agreement and < 15% disagreement, or vice versa).HCP = healthcare professional; IGRT = image-guided radiotherapy; IMRT = intensity-modulated radiotherapy;5FU = 5-fluorouracil; MMC = mitomycin-C.
7.6. Adjuvant therapy
7.6.1. Role of adjuvant platinum-based chemotherapy
Adjuvant chemotherapy after RC for patients with pT3/4 and/or LN positive (N+) disease without clinically detectable metastases (M0) is still under debate [445,446]. The general benefits of adjuvant chemotherapy include:
- chemotherapy is administered after accurate pathological staging, therefore, treatment in patients at low risk for micrometastases is avoided;
- no delay in definitive surgical treatment.
The drawbacks of adjuvant chemotherapy are:
- assessment of in vivo chemosensitivity of the tumour is not possible and overtreatment is an unavoidable problem;
- delay of or intolerability to chemotherapy, due to post-operative morbidity [447].
There is limited evidence from adequately conducted and accrued phase III RCTs in favour of the routine use of adjuvant chemotherapy [446,448-453]. An individual patient data meta-analysis [503] of survival data from six RCTs of adjuvant chemotherapy [454-458] included 491 patients (unpublished data from Otto et al., were included in the analysis). All included trials suffered from significant methodological flaws including small sample size (underpowered), incomplete accrual, use of inadequate statistical methods and design flaws (irrelevant endpoints and failing to address salvage chemotherapy in case of relapse or metastases) [446]. In these trials, three or four cycles of CMV, cisplatin, cyclophosphamide, and adriamycin (CISCA), methotrexate, vinblastine, adriamycin or epirubicin, and cisplatin (MVA(E)C) and cisplatin with methotrexate (CM) were used [459], and one trial used cisplatin monotherapy [457]. The data were not convincing to support an unequivocal recommendation for the use of adjuvant chemotherapy. In 2014, this meta-analysis was updated with an additional three studies [450-452] resulting in the inclusion of 945 patients from nine trials [449]. None of the trials had fully accrued and individual patient data were not used in the analysis [449]. For one trial only an abstract was available at the time of the meta-analysis [451] and none of the included individual trials were significantly positive for OS in favour of adjuvant chemotherapy. In two of the trials more modern chemotherapy regimens were used (gemcitabine/cisplatin and paclitaxel/gemcitabine/cisplatin) [450,451]. The HR for OS was 0.77 (95% CI: 0.59–0.99, p = 0.049) and for DFS 0.66 (95% CI: 0.45–0.91, p = 0.014) with a stronger impact on DFS in case of nodal positivity. Recently, a systematic review and meta-analysis of individual patient data from RCTs in patients treated with adjuvant cisplatin-based chemotherapy for MIBC was conducted [460]. In an analysis of 10 RCTs (n = 1,183), an OS benefit was demonstrated for cisplatin-based adjuvant chemotherapy (HR: 0.82, 95% CI: 0.70–0.96, p = 0.02). This translates into an absolute improvement in survival of 6% at 5 years, from 50% to 56%, and a 9% absolute benefit when adjusted for age, sex, pT stage, and pN category (HR: 0.77, 95% CI: 0.65–0.92, p = 0.004). Adjuvant chemotherapy was also shown to improve RFS (HR: 0.71, 95% CI: 0.60-0.83, p < 0.001), locoregional RFS (HR: 0.68, 95% CI: 0.55–0.85, p < 0.001), and MFS (HR: 0.79, 95% CI: 0.65–0.95, p = 0.01), with absolute benefits of 11%, 11%, and 8%, respectively.
A retrospective cohort analysis including 3,974 patients after cystectomy and LND showed an OS benefit in high-risk subgroups (extravesical extension and nodal involvement) (HR: 0.75, CI: 0.62–0.90) [461]. A recent publication of the largest RCT (European Organisation for Research and Treatment of Cancer [EORTC] 30994), although not fully accrued, showed a significant improvement of PFS for immediate, compared with deferred, cisplatin-based chemotherapy (HR: 0.54, 95% CI: 0.4–0.73, p < 0.0001), but there was no significant OS benefit [462].
Furthermore, a large observational study including 5,653 patients with pathological T3–4 and/ or pathological node-positive BC, treated between 2003 and 2006 compared the effectiveness of adjuvant chemotherapy vs. observation. Twenty-three percent of patients received adjuvant chemotherapy with a 5-year OS of 37% for the adjuvant arm vs. 29.1% (HR: 0.70, 95% CI: 0.64–0.76) in the observation group [463]. Another large retrospective analysis based on the U.S. National Cancer Database including 15,397 patients with locally-advanced (pT3/4) or LN-positive disease also demonstrated an OS benefit in patients with UC histology [464]. In patients with concomitant histological subtypes, however, no benefit was found.
Patients should be informed about potential chemotherapy options before RC and the limited evidence for adjuvant chemotherapy.
7.6.2. Role of adjuvant immunotherapy
To determine the benefit of PD-1/PD-L1 checkpoint inhibitors, three phase III RCTs have evaluated checkpoint inhibitor monotherapy with atezolizumab, nivolumab or pembrolizumab in patients with muscle-invasive UC. The CheckMate 274 phase III multi-centre, double-blind, RCT of adjuvant nivolumab vs. placebo for up to
1 year in 709 patients with muscle-invasive UC with a high risk of recurrence (pathological stage pT3, pT4a, or pN+) (neoadjuvant cisplatin-based chemotherapy was allowed before trial entry) demonstrated a significant improvement in median DFS (20.8 months [95% CI: 16.5–27.6] with nivolumab and 10.8 months [95%
CI: 8.3–13.9] with placebo). The percentage of patients who were alive and disease-free at 6 months
was 74.9% with nivolumab and 60.3% with placebo (HR for disease recurrence or death, 0.70; 98.22%
CI: 0.55–0.90; p < 0.001). Among patients with a PD-L1 expression level of > 1%, the percentage of patients was 74.5% and 55.7%, respectively (HR: 0.55; 98.72% CI: 0.35–0.85; p < 0.001) [465].
The primary endpoint of DFS was not achieved in a multi-centre RCT of adjuvant atezolizumab vs. observation in patients with ypT2–4a or ypN+ tumours following NAC or pT3–4a or pN+ tumours if no NAC was received (IMvigor010). Median DFS was 19.4 months (95% CI: 15.9–24.8) with atezolizumab and 16.6 months (11.2–24.8) with observation (stratified HR: 0.89, 95% CI: 0.74–1.08, p = 0.24) [466]. A similarly designed trial of pembrolizumab in the adjuvant setting has completed accrual with results awaited.
The FDA has approved nivolumab for adjuvant treatment of patients with UC who are at high risk of recurrence after undergoing surgery [467] whereas the EMA has approved adjuvant nivolumab for the treatment of adults with muscle-invasive UC (MIUC) with tumour cell PD-L1 expression > 1%, who are at high risk of recurrence after undergoing radical resection of MIUC. A promising report (see Marker section) has suggested a potential role for ctDNA to guide the use of adjuvant IO for UC [468].
7.6.3. Summary of evidence and guidelines for adjuvant therapy
Summary of evidence | LE |
Adjuvant cisplatin-based chemotherapy for high-risk patients (pT3, 4 and/or or N+ M0) without neoadjuvant treatment can be associated with improvement in DFS and OS but trials are underpowered to adequately answer this question. | 2a |
To date, studies of immune checkpoint inhibitors in the adjuvant setting in patients with high-risk | 1b |
Circulating tumour DNA holds promise as both a prognostic and predictive biomarker to guide the use of adjuvant IO for UC in patients who are at a high risk of recurrence and positive for ctDNA treated with adjuvant atezolizumab demonstrating improved outcomes compared with observation. | 2b |
Recommendations | Strength rating |
Offer adjuvant cisplatin-based combination chemotherapy to patients with pT3/4 and/or pN+ disease if no neoadjuvant chemotherapy has been given. | Strong |
Offer adjuvant nivolumab to selected patients with pT3/4 and/or pN+ disease not eligible for, or who declined, adjuvant cisplatin-based chemotherapy. | Weak |
7.7. Metastatic disease
7.7.1. Introduction
The treatment of metastatic UC had remained largely unchanged since pivotal trials published over 20 years ago set the standard of care for first-line treatment with cisplatin-based combinations demonstrating an OS benefit. In the past few years this long-standing paradigm has been challenged by several large studies investigating the benefit of immunotherapy using checkpoint inhibitors. Moreover, novel compounds including both targeted therapy and antibody-drug conjugates have been successfully tested and approved in later treatment lines.
7.7.2. First-line systemic therapy for metastatic disease
In general, patients with untreated metastatic UC can be divided into three broad categories: fit for cisplatin-based chemotherapy, fit for carboplatin-based chemotherapy (but unfit for cisplatin) and unfit for any platinum-based chemotherapy.
Definitions: ‘Fit for cisplatin, fit for carboplatin, unfit for any platinum-based chemotherapy’
An international survey among BC experts [469] was the basis for a consensus statement on how to classify patients unfit for cisplatin-based chemotherapy. At least one of the following criteria must be present: PS > 1; GFR < 60 mL/min; grade > 2 audiometric hearing loss; grade > 2 peripheral neuropathy or New York Heart Association (NYHA) class III heart failure [470]. Around 50% of patients with BC are not eligible for cisplatin-based chemotherapy [470]. Renal function assessment is of utmost importance for treatment selection. Measuring GFR with radioisotopes (99mTc DTPA or 51Cr-EDTA) is recommended in equivocal cases.
Cisplatin has also been administered in patients with a lower GFR (40–60 mL/min) using different split-dose schedules. The respective studies were mostly small phase I and II trials in different settings (neoadjuvant and advanced disease) demonstrating that the use of split-dose cisplatin is feasible and appears to result in encouraging efficacy [468,471,472]. However, no prospective RCT has compared split-dose cisplatin with conventional dosing.
Most patients that are deemed unfit for cisplatin are able to receive carboplatin-based chemotherapy. However, some patients are deemed unfit for any platinum-based chemotherapy, i.e. both cisplatin and carboplatin. Patient are unfit for any platinum-based chemotherapy in case of PS > 2, GFR < 30 mL/min or the combination of PS 2 and GFR < 60 mL/min since the outcome in this patient population is poor regardless of platinum-based treatment or not [473]. Patients with multiple comorbidities may also be poor candidates for platinum-based chemotherapy. Definitions of platinum-eligibility for first-line treatment of metastatic UC are summarised in Table 7.2.
Table 7.2: Definitions of platinum-eligibility for first-line treatment of metastatic urothelial carcinoma
Platinum-eligible | Platinum-ineligible | |
Cisplatin-eligible | Carboplatin-eligible | |
ECOG PS 0-1 and | ECOG PS 2 or GFR 30–60 mL/min | Any of the following: |
GFR > 50–60 mL/min and | or not fulfilling other cisplatin-eligibility criteria | GFR < 30 mL/min |
Audiometric hearing loss grade < 2 | ECOG PS > 2 | |
Peripheral neuropathy grade < 2 and | ECOG PS 2 and GFR < 60 mL/min | |
Cardiac insufficiency NYHA class < III | Comorbidites > Grade 2 | |
ECOG = Eastern Cooperative Oncology Group; GFR = glomerular filtration rate; NYHA = New York HeartAssociation; PS = performance status.
7.7.2.1. First-line chemotherapy in patients fit for cisplatin
Cisplatin-containing combination chemotherapy has been the standard of care since the late 1980s demonstrating an OS of 12 to 14 months in different series (for a review see [474]). Methotrexate, vinblastine, adriamycin plus cisplatin and GC achieved survival of 14.8 and 13.8 months, respectively [475]. Overall response rates were 46% for MVAC and 49% for GC. The lower toxicity of GC [204] compared to standard MVAC has resulted in GC becoming the standard regimen.
Dose-dense MVAC combined with granulocyte colony-stimulating factor (G-CSF) is less toxic and more efficacious than standard MVAC in terms of, complete response (CR), and 2-year OS. However, there is no significant difference in median survival between the two regimens [476,477]. Further intensification of treatment using paclitaxel, cisplatin and gemcitabine (PCG) triple regimen did not result in a significant improvement in OS in the intention-to-treat (ITT) population of a phase III RCT, comparing PCG to GC [478]. Similarly, the addition of the angiogenesis inhibitor bevacizumab to GC did not result in OS improvement [479].
The disease sites have an impact on long-term survival. In LN-only disease, 20.9% of patients were alive at five years compared to only 6.8% of patients with visceral metastases [475]. In the trials with long-term follow-up approximately 10-15% of patients with metastatic UC are alive at 5 years and longer, suggesting a sustained benefit from cisplatin-based chemotherapy in a minority of patients [475,477].
Carboplatin-containing chemotherapy is not considered to be equivalent to cisplatin-based combinations, and should not be considered interchangeable or standard in patients fit for cisplatin. A comparative analysis of four randomised phase II trials of carboplatin vs. cisplatin combination chemotherapy demonstrated lower CR rates and shorter OS for the carboplatin arms [480]. Recently, a retrospective study highlighted the importance of applying cisplatin in cisplatin-eligible patients in order to maintain benefit [481].
7.7.2.2. First-line chemotherapy in patients fit for carboplatin (but unfit for cisplatin)
Up to 50% of patients are not fit for cisplatin-containing chemotherapy but most may be candidates for carboplatin [470]. The first randomised phase II/III trial in this setting was conducted by the EORTC and compared two carboplatin-containing regimens (methotrexate/carboplatin/vinblastine [M-CAVI] and gemcitabine / carboplatin [GemCarbo]) in patients unfit for cisplatin. The EORTC definitions for eligibility were GFR < 60 mL/min and/or PS 2. Severe acute toxicity was 13.6% with GemCarbo vs. 23% with M-CAVI, while the ORR was 42% for GemCarbo and 30% for M-CAVI, respectively [473]. Based on these results the combination of carboplatin and gemcitabine should be considered a standard of care in this patient group.
Combinations of gemcitabine and paclitaxel have been studied as first-line treatment and produced response rates between 38% and 60% but has never been tested in RCTs [482-484]. A randomised phase II trial assessed the efficacy and tolerability profile of two vinflunine-based regimens (vinflunine/gemcitabine vs. vinflunine/carboplatin). Both regimens showed equal ORR and OS with less haematologic toxicity for the combination of vinflunine/gemcitabine [485]. Non-platinum combination chemotherapy is nevertheless not recommended for first-line use in platinum-eligible patients.
The use of single-agent chemotherapy has been associated with varying response rates. Responses with single agents are usually short, complete responses are rare, and no long-term DFS/OS has been reported. It is not recommended for first-line treatment of metastatic UC.
7.7.2.3. Integration of immunotherapy in the first-line chemotherapy treatment of patients fit for platinum (cisplatin or carboplatin)
7.7.2.3.1. Immunotherapy combination approaches
In 2020, the results of three phase III trials have been published investigating the use of immunotherapy in the first-line setting for platinum-eligible patients. The first trial to report was IMvigor130 investigating the combination of the PD-L1 inhibitor atezolizumab plus platinum-gemcitabine chemotherapy vs. chemotherapy plus placebo vs. atezolizumab alone [486]. The primary endpoint of PFS benefit for the combination vs. chemotherapy alone in the ITT group was reached (8.2 months vs. 6.3 months [HR: 0.82, 95% CI: 0.70–0.96; one-sided, p = 0.007]) while OS was not significant at the interim analysis after a median follow-up of 11.8 months. The small PFS benefit in the absence of an OS benefit has raised questions of its clinical significance. Due to the sequential testing design, the comparison of chemotherapy vs. atezolizumab alone has not yet been formally performed.
The KEYNOTE 361 study had a very similar design using the PD-1 inhibitor pembrolizumab plus platinum-gemcitabine vs. chemotherapy plus placebo vs. pembrolizumab alone. The results of the primary endpoints of PFS and OS for the comparison of pembrolizumab plus chemotherapy vs. chemotherapy plus placebo in the ITT population showed no benefit for the combination [487].
DANUBE compared the immunotherapy combination (IO-IO) of CTLA-4 inhibitor tremelimumab and PD-L1 inhibitor durvalumab with chemotherapy alone or durvalumab alone [488]. The co-primary endpoint of improved OS for the IO-IO combination vs. chemotherapy was not reached in the ITT group nor was the OS improved for durvalumab monotherapy vs. chemotherapy in the PD-L1-positive population.
In conclusion, these three trials do not support the use of combination of PD-1/L1 checkpoint inhibitors plus chemotherapy or the IO-IO combination as first-line treatment.
7.7.2.3.2. Use of first-line single-agent immunotherapy in patients unfit for cisplatinum-based chemotherapy
Based on the results of two single-arm phase II trials [489,490] the checkpoint inhibitors pembrolizumab and atezolizumab have been approved by the U.S. FDA and the EMA for first-line treatment in cisplatin-unfit patients in case of positive PD-L1 status. PD-L1 positivity for use of pembrolizumab is defined by immunohistochemistry as a CPS of > 10 using the Dako 22C33 platform and for atezolizumab as positivity of
> 5% tumour-infiltrating immune cells using Ventana SP142.
Pembrolizumab was tested in 370 patients with advanced or metastatic UC ineligible for cisplatin, showing an ORR of 29% and CR in 7% of patients [489]. Atezolizumab was evaluated in the same patient population in a phase II trial (n = 119) showing an ORR of 23% with 9% of patients achieving CR [490].
The trials IMvigor 130, Keynote 361 and DANUBE all included an experimental arm with immunotherapy alone using atezolizumab, pembrolizumab and durvalumab, respectively [486-488]. No benefit in terms of PFS or OS for the use of single-agent immunotherapy compared to platinum-based chemotherapy was found. The combination of carboplatin/gemcitabine therefore is considered the preferred first-line treatment choice for patients ineligible for cisplatin but eligible for carboplatin.
7.7.2.3.3. Switch maintenance with immunotherapy after platinum-based chemotherapy
A randomised phase II trial evaluated switch maintenance treatment with pembrolizumab in patients achieving at least stable disease on platinum-based first-line chemotherapy. The primary endpoint of PFS was met (5.4 months vs. 3.0 months, HR: 0.65, p = 0.04) but not the secondary endpoint of OS (22 months vs. 18.7 months, HR: 0.91, 95% CI: 0.52–1.59) [491].
The JAVELIN Bladder 100 study investigated the impact of switch maintenance with the PD-L1 inhibitor avelumab after initial treatment with platinum-gemcitabine chemotherapy. Patients achieving at least stable disease or better after 4–6 cycles of platinum-gemcitabine were randomised to avelumab or best supportive care (BSC). Overall survival was the primary endpoint which improved to 21.4 months with avelumab compared to 14.3 months with BSC (HR: 0.69, 95% CI: 0.56–0.86; p < 0.001). Of patients who discontinued BSC and received subsequent treatment 53% received immunotherapy. Immune-related AEs occurred in 29% of all patients and 7% experienced grade 3 complications [492].
In conclusion, maintenance IO with avelumab is a standard of care for all patients with disease stabilisation on first-line platinum-based chemotherapy.
7.7.2.4. Treatment of patients unfit for any platinum-based chemotherapy
Very limited data exist regarding the optimal treatment for this patient population which is characterised by severely impaired PS (PS > 2) and/or severely impaired renal function (GFR < 30 mL/min). Historically, the outcome in this patient group has been poor. Best supportive care has often been chosen instead of systemic therapy. Most trials evaluating alternative treatment options to cisplatinum-based chemotherapy did not focus specifically on this patient population thereby making interpretation of data difficult. The FDA (but not EMA) has approved pembrolizumab and atezolizumab as first-line treatment for patients not fit to receive any platinum-based chemotherapy regardless of PD-L1 status based on the results of two single-arm phase II trials [489,490]. These trials have not reported how many patients were unfit for any platinum-based chemotherapy.
7.7.3. Second-line systemic therapy for metastatic disease
7.7.3.1. Second-line chemotherapy
Second-line chemotherapy data are highly variable and mainly derive from small single-arm phase II trials apart from a single phase III RCT. A reasonable strategy has been to re-challenge former platinum-sensitive patients if progression occurred at least six to twelve months after first-line platinum-based combination chemotherapy. A retrospective analysis of 296 patients within the the RISC cohort (Retrospective International Study of Cancers of the Urothelium) revealed that subsequent platinum-based combination chemotherapy achieved a somewhat higher disease control rate (57.4% vs. 44.8%, p.= 0.041) and OS (7.9 vs. 5.5 months, p = 0.035) compared to subsequent non-platinum-based chemotherapy [493]. Second-line response rates of single-agent treatment with paclitaxel (weekly), docetaxel, gemcitabine, nab-paclitaxel, oxaliplatin, ifosfamide, topotecan, pemetrexed, lapatinib, gefitinib and bortezomib have ranged between 0% and 28% in small phase II trials [494,495].
The paclitaxel/gemcitabine combination has shown good response rates in small single-arm studies but no adequate phase III RCT has been conducted [496,497].
Vinflunine was tested in a phase III RCT and compared against BSC in patients progressing after first-line treatment with platinum-based chemotherapy [498]. The results showed a very modest ORR (8.6%), a clinical benefit with a favourable safety profile and a survival benefit, which was however only statistically significant in the eligible patient population (not in the ITT population).
A randomised phase III trial evaluated the addition of the angiogenesis inhibitor ramucirumab to docetaxel chemotherapy vs. docetaxel alone, which resulted in improved PFS (4.1 vs. 2.8 months) and higher response rates (24.5% vs. 14%) but no OS benefit was achieved [499,500].
7.7.3.2. Second-line immunotherapy for platinum-pre-treated patients
The immune checkpoint inhibitors pembrolizumab, nivolumab, atezolizumab, avelumab, and durvalumab have demonstrated similar efficacy and safety in patients progressing during, or after, previous platinum-based chemotherapy in phase I, II and III trials.
Pembrolizumab demonstrated a significant OS Improvement as second-line treatment in a phase III RCT leading to EMA and FDA approval. Patients (n = 542) were randomised to receive either pembrolizumab monotherapy or chemotherapy (paclitaxel, docetaxel or vinflunine). The median OS with pembrolizumab was 10.3 months (95% CI: 8.0–11.8) vs. 7.4 months (95% CI: 6.1–8.3) with chemotherapy (HR 0.73, 95% CI: 0.59–0.91, p = 0.002) independent of PD-L1 expression levels [501].
Atezolizumab was the first checkpoint inhibitor approved by the FDA for metastatic UC based on the results of phase I and II trials [236,502] The phase III RCT (IMvigor211) included 931 patients comparing atezolizumab with second-line chemotherapy (paclitaxel, docetaxel or vinflunine) did not meet its primary endpoint of improved OS for patients with high PD-L1 expression with 11.1 months (atezolizumab) vs. 10.6 (chemotherapy) months (stratified HR: 0.87, 95% CI: 0.63–1.21, p = 0.41) [503].
The PD-1 inhibitor nivolumab was approved by the FDA based on the results of a single-arm phase II trial (CheckMate 275), enrolling 270 platinum pre-treated patients. The primary endpoint of ORR was 19.6%, and OS was 8.74 months for the entire group [504].
Based on level 1 evidence from a RCT, pembrolizumab has emerged in clinic as the preferred standard of care immunotherapy in the second-line setting.
7.7.3.3. Side-effect profile of immunotherapy
Checkpoint inhibitors including PD-1 or PD-L1 antibodies and CTLA-4 antibodies have a distinct side-effect profile associated with their mechanism of action leading to enhanced immune system activity. These AEs can affect any organ in the body leading to mild, moderate or severe side effects. The most common organs affected are the skin, GI tract, liver, lung, thyroid, adrenal and pituitary gland. Other systems that may be affected include musculoskeletal, renal, nervous, haematologic, ocular and cardiovascular system. Any change during immunotherapy treatment should raise suspicion about a possible relation to the treatment. The nature of immune-related AEs has been very well characterised and published [505]. The timely and appropriate treatment of immune-related side effects is crucial to achieve optimal benefit from the treatment while maintaining safety. Clear guidelines for side-effect management have been published [506]. Immunotherapy treatment should be applied and supervised by trained clinicians only to ensure early side effect recognition and treatment. In case of interruption of immunotherapy, re-challenge will require close monitoring for
AEs [507].
7.7.4. Integration of novel agents
7.7.4.1. Antibody drug conjugates
The first antibody drug conjugate to report encouraging data was enfortumab vedotin, an antibody-drug conjugate targeting Nectin-4, a cell adhesion molecule which is highly expressed in UC conjugated to monomethyl auristatin E (MMAE). A phase-II single-arm study (EV-201) in 125 patients previously treated with platinum chemotherapy and checkpoint inhibition showed a confirmed objective response rate of 44%, including 12% complete responses [508]. This data led to accelerated FDA and EMA approval for enfortumab vedotin in locally-advanced or metastatic UC patients who previously received a PD-1 or PD-L1 inhibitor and platinum-containing chemotherapy, as well as for cisplatin-ineligible patients who received one or more prior lines of therapy [509,510]. Another cohort of the same EV-201 trial demonstrated similar promising results in a cohort of 91 patients that were cisplatin-ineligible and had received prior IO [511]. A phase III RCT (n = 608) comparing enfortumab vedotin with single-agent chemotherapy after prior platinum chemotherapy and checkpoint inhibitor immunotherapy demonstrated significant survival benefit of almost 4 months (12.88 months vs. 8.97 months; HR 0.7, 95% CI: 0.56–0.89) [512]. The most common treatment-related AEs included alopecia (45%), peripheral neuropathy (34%), fatigue (31%, 7.4% > grade 3), decreased appetite (31%), diarrhoea (24%), nausea (23%) and skin rash (16%, 7.4% > grade 3).
The combination of enfortumab vedotin and pembrolizumab as first-line treatment in 45 cisplatin-ineligible patients with locally-advanced/metastatic UC demonstrated a confirmed objective response rate after a median of nine cycles of 73.3% with a complete response rate of 15.6%. The median duration of response and median OS were 25.6 months and 26.1 months, respectively. The most common treatment-related AEs were peripheral sensory neuropathy (55.6%), fatigue (51.1%), and alopecia (48.9%) [513]. Based on these results enfortumab vedotin has been FDA approved for patients who received prior platinum-containing chemotherapy and prior IO with PD-1 or PD-L1 inhibitor as well as for cisplatin-ineligible patients who received one or more prior lines of therapy. An ongoing randomised phase III study is investigating the potential role for the combination of enfortumab vedotin and pembrolizumab in the first-line setting for patients with metastatic disease (EV-302: NCT04223856).
Another new and also promising antibody drug conjugate is sacituzumab govitecan, consisting of a humanised monoclonal antibody targeting trophoblast cell surface antigen 2 (Trop-2) conjugated to SN-38, the active metabolite of irinotecan. Sacituzumab govitecan was tested in 113 platinum and IO pre-treated metastatic UC (mUC) patients [508] and achieved an ORR of 27% and a total of 77% had a decrease in measurable disease, median PFS was 5.4 months and median OS 10.9 months [514]. Side effects consisted of haematological toxicities (neutropenia 34% > grade 3; febrile neutropenia 10% > grade 3), fatigue (52%), alopecia (47%), nausea (60%), diarrhea (65%, 10% > grade 3) and decreased appetite (36%) [514]. Sacituzumab govitecan has received accelerated FDA approval for metastatic UC with prior platinum and IO pre-treatment. Several trials using sacituzumab govitecan as monotherapy or in combination are ongoing.
7.7.4.2. FGFR inhibition
Genomic profiling of UC has revealed common potentially actionable genomic alterations including alterations in FGFR [515]. Erdafitinib is a pan-FGFR tyrosine kinase inhibitor and the first FDA-approved targeted therapy for mUC with susceptible FGFR2/3 alterations following platinum-containing chemotherapy. The phase II trial of erdafitinib included 99 patients whose tumour harboured an FGFR3 mutation or FGFR2/3 fusion and who had disease progression following chemotherapy [234]. The confirmed ORR was 40% and an additional 39% of patients had stable disease. A total of 22 patients had previously received immunotherapy with only one patient achieving a response, yet the response rate for erdafitinib for this subgroup was 59%. At a median follow-up of 24 months, the median PFS was 5.5 months (95% CI: 4.0–6.0) and the median OS was 11.3 months (95% CI: 9.7–15.2) [234]. Treatment-related AEs of > grade 3 occurred in 46% of patients. Common AEs of > grade 3 were hyponatraemia (11%), stomatitis (10%), and asthenia (7%) and 13 patients discontinued erdafitinib due to AEs, including retinal pigment epithelial detachment, hand-foot syndrome, dry mouth, and skin/nail events. In addition to erdafitinib, several other FGFR inhibitors are being evaluated including infigratinib which has demonstrated promising activity [235]. In the recently published long-term follow up, the efficacy and safety profile remained similar with no new safety signals with longer follow-up [516]. The increased identification of FGFR3 mutations/fusion has led to several ongoing trials with different agents and combinations in different disease settings.
7.7.5. Current status of predictive biomarkers
The most important advance in recent years has been the recognition of alterations in FGFR3 including mutations and gene fusions as a predictive marker for response to FGFR inhibitors [234]. It is recommended to screen mUC patients ideally at diagnosis of metastatic disease for FGFR3 alterations to plan optimal treatment including trials.
Many efforts have focused on markers for predicting response to immune checkpoint inhibition. Programmed death-ligand 1 expression by immunohistochemistry has been evaluated in many studies with mixed and, so far, inconclusive results. This may in part be related to the use of different antibodies and various scoring systems evaluating different compartments i.e., tumour cells, immune cells, or both. A major limitation of PD-L1 staining relates to the significant proportion of PD-L1-negative patients that respond to immune checkpoint blockade. The predictive value of PD-L1 was not confirmed in large phase III trials evaluating the integration of immunotherapy in the first-line setting for mUC [486-488]. At present, the only indication for PD-L1 testing in mUC is dictated by current FDA and EMA approvals and relates to the potential use of immune checkpoint inhibitors as first-line monotherapy in patients unfit for cisplatin-containing chemotherapy.
Another biomarker that has been evaluated for predicting response to immunotherapy is high TMB [238]. Neoantigen burden and TMB have been associated with response to immune checkpoint blockade in several malignancies. High TMB has been associated with response to immune checkpoint inhibitors in metastatic UC in small single-arm trials [236,239] but was not confirmed so far in RCTs. Other markers that have been evaluated in predicting response to immune checkpoint inhibitors include molecular subtypes, CD8 expression by immunohistochemistry and other immune gene cell signatures. Recent work has focused on the importance of stroma including the role of TGFs in predicting response to immune checkpoint blockade [242,243].
In conclusion, apart from FGFR3 alterations, there are currently no further validated predictive molecular markers that are routinely used in clinical practice.
7.7.6. Special situations
7.7.6.1. Impact of prior neoadjuvant/adjuvant therapy on treatment sequence
Peri-operative systemic treatment is increasingly used in UC including cisplatin-based chemotherapy in the neoadjuvant setting for BC and adjuvant platinum-based chemotherapy for upper tract UC [517]. Many ongoing phase III trials investigate the use of immunotherapy in this setting as well (see Section 7.6.2). So far, one trial has reported a significant DFS benefit for adjuvant treatment with nivolumab compared with placebo whereas one trial reported no significant benefit using atezolizumab vs. placebo in the same setting whilst another trial reported negative findings [465,466]. It is expected that an increased number of patients with metastatic UC will have received pre-treatment with platinum and/or immunotherapy agents. No prospective trials have investigated the treatment of such patients. The choice of treatment in these patients depends on the applied peri-operative treatment and the time until relapse. If at least 12 months have passed since the end of peri-operative treatment the same systemic treatment as in treatment-naive patients is recommended. To help prevent early relapse within 12 months the peri-operative systemic therapy has to be taken into account when planning further treatment.
7.7.6.2. Systemic treatment of metastatic disease with histology other than pure urothelial carcinoma
Pure UC represents the predominant histology in over 90% of patients with mUC. Variant histologies (e.g. micropapillary, nested, sarcomatoid) and divergent differentiation (e.g., SCC, adenocarcinoma) can be found in addition to pure UC in up to 33% of patients. Such patients were often excluded from large phase II and phase III trials and therefore the knowledge about the best management of such patients is limited. The respective literature was reviewed recently [69] and an expert Delphi survey and consensus conference provided guidance [10]. In case of predominant pure UC it is recommended to treat patients with mixed histology the same way as patients with a pure UC histology. Patients with predominant non-urothelial differentiation such as small cell neuroendocrine carcinoma, urachal adenocarcinoma, SCC and adenocarcinoma should be treated individually.
7.7.7. Treatment of patients with bone metastases
The prevalence of metastatic bone disease (MBD) in patients with advanced/metastatic UC is 30–40% [518]. Interestingly, a recent report described several observations related to age- and sex-related differences in the distribution of metastases in patients with metastatic BC and demonstrated that bone was the most common metastatic site in men with other differences noted according to patient age and sex [519]. Skeletal complications due to MBD have a detrimental effect on pain and QoL and are also associated with increased mortality [520]. Bisphosphonates such as zoledronic acid reduce and delay skeletal-related events (SREs) due to bone metastases by inhibiting bone resorption, as shown in a small pilot study [521]. Denosumab, a fully human monoclonal antibody that binds to and neutralises RANKL (receptor activator of nuclear factor κB ligand), was shown to be non-inferior to zoledronic acid in preventing or delaying SREs in patients with solid tumours and advanced MBD, including patients with UC [522]. Patients with MBD, irrespective of the cancer type, should be considered for bone-targeted treatment [520].
Patients treated with zoledronic acid or denosumab should be informed about possible side effects including osteonecrosis of the jaw and hypocalcaemia. Supplementation with calcium and vitamin D is mandatory. Dosing regimens of zoledronic acid should follow regulatory recommendations and have to be adjusted according to pre-existing medical conditions, especially renal function [523]. For denosumab, no dose adjustments are required for variations in renal function.
7.7.8. Summary: treatment algorithm for metastatic urothelial cancer update 2021
Figure 7.2 summarises the treatment algorithm for metastatic BC based on the evidence discussed in the text above.
Patients with treatment-naive mUC are grouped according to platinum-eligibility based on clear definitions. In general, first-line treatment consists of platinum-based chemotherapy in which cisplatin is to be preferred to carboplatin. Patients who are cisplatin-ineligible but carboplatin-eligible should receive gemcitabine-carboplatin combination chemotherapy. In case of positive PD-L1 status, treatment with checkpoint inhibitors (atezolizumab or pembrolizumab) could be an alternative option.
Patients unfit for both cisplatin and carboplatin (platinum-unfit) can be considered for immunotherapy (FDA approved irrespective of PD-L1 status, EMA approved only for PD-L1 positive patients) or receive BSC.
In cases of disease stabilization on platinum-based chemotherapy switch, maintenance treatment with IO (avelumab) is recommended. Alternatively, patients can be followed closely and receive second-line immunotherapy at the time of progression (pembrolizumab).
It is recommended to determine FGFR mutation status before deciding about second-line treatment. Patients with FGFR3 mutations are candidates for FGFR inhibitor treatment. Enfortumab vedotin therapy is the new standard in case of progression after platinum chemotherapy and IO but has not yet been approved in Europe. The optimal sequence of novel agents and potential combinations are the subject of many ongoing trials. It is generally recommended to treat patients within ongoing clinical trials.
7.7.9. Summary of evidence and guidelines for metastatic disease
Summary of evidence | LE |
In a first-line setting, PS and the presence or absence of visceral metastases are independent prognostic factors for survival. | 1b |
In a second-line setting, negative prognostic factors are: liver metastasis, PS > 1 and low haemoglobin (< 10 g/dL). | 1b |
Cisplatin-containing combination chemotherapy can achieve median survival of up to 14 months, with long-term DFS reported in ~15% of patients with nodal disease and good PS. | 1b |
Single-agent chemotherapy provides low response rates of usually short duration. | 2a |
Carboplatin combination chemotherapy is less effective than cisplatin-based chemotherapy in terms of complete response and survival. | 2a |
There is no defined standard therapy for platinum chemotherapy-unfit patients with advanced or metastatic UC. | 2b |
Post-chemotherapy surgery after partial or complete response may contribute to long-term DFS in highly selected patients. | 3 |
Zoledronic acid and denosumab have been approved for supportive treatment in case of bone metastases of all cancer types including UC, as they reduce and delay skeletal related events. | 1b |
PD-1 inhibitor pembrolizumab has been approved for patients that have progressed during or after previous platinum-based chemotherapy based on the results of a phase III trial. | 1b |
Enfortumab vedotin after prior platinum chemotherapy and checkpoint inhibitor immunotherapy has demonstrated a significant survival benefit as compared to chemotherapy. | 1b |
PD-1 inhibitor atezolizumab is approved for patients with advanced or metastatic UC unfit for cisplatin-based chemotherapy in case of high PD-L1 expression defined as tumour-infiltrating immune cells covering > 5% of the tumour area using the SP142 assay. | 1b |
PD-1 inhibitor pembrolizumab is approved for patients with advanced or metastatic UC unfit for any platinum-based chemotherapy in case of high PD-L1 expression defined as CPS of > 10 using the Dako 22C33 platform (EMA; FDA approval independent of PD-L1 status). | 1b |
The combination of chemotherapy plus pembrolizumab or atezolizumab and the combination of durvalumab and tremelimumab have not demonstrated OS survival benefit compared to platinum-based chemotherapy alone. | 1b |
Switch maintenance with the PD-L1 inhibitor avelumab has demonstrated significant OS benefit in patients achieving at least stable disease on first-line platinum-based chemotherapy. | 1b |
Recommendations | Strength rating |
First-line treatment for platinum-fit patients | |
Use cisplatin-containing combination chemotherapy with GC or HD-MVAC. | Strong |
In patients unfit for cisplatin but fit for carboplatin, use the combination of carboplatin and gemcitabine. | Strong |
In patients achieving stable disease, or better, after first-line platinum-based chemotherapy, use maintenance treatment with PD-L1 inhibitor avelumab. | Strong |
First-line treatment in patients unfit for platinum-based chemotherapy | |
Consider checkpoint inhibitors pembrolizumab or atezolizumab in case of high PD-L1 expression (for definitions see text). | Weak |
Second-line treatment | |
Offer checkpoint inhibitor pembrolizumab to patients progressing during, or after, platinum-based combination chemotherapy for metastatic disease. | Strong |
Further treatment after platinum- and immunotherapy | |
Offer antibody drug conjugate enfortumab vedotin as monotherapy to patients with advanced or metastatic UC pre-treated with platinum and immunotherapy. | Strong |
Offer treatment in clinical trials testing novel drugs (e.g. sacituzumab govitecan); or in case of patients with FGFR3 alterations, FGFR tyrosine kinase inhibitors. | Strong |
Evaluate for FGFR2/3 genetic alterations for the potential use of erdafitinib in patients with locally-advanced or metastatic urothelial carcinoma who have progressed following platinum-containing chemotherapy (including within 12 months of neoadjuvant or adjuvant platinum-containing chemotherapy). | Weak |
GC = gemcitabine plus cisplatin; FGFR = fibroblast growth factor receptor; HD-MVAC = high-dose intensitymethotrexate, vinblastine, adriamycin plus cisplatin.
Figure 7.2: Flow chart for the management of metastatic urothelial cancer*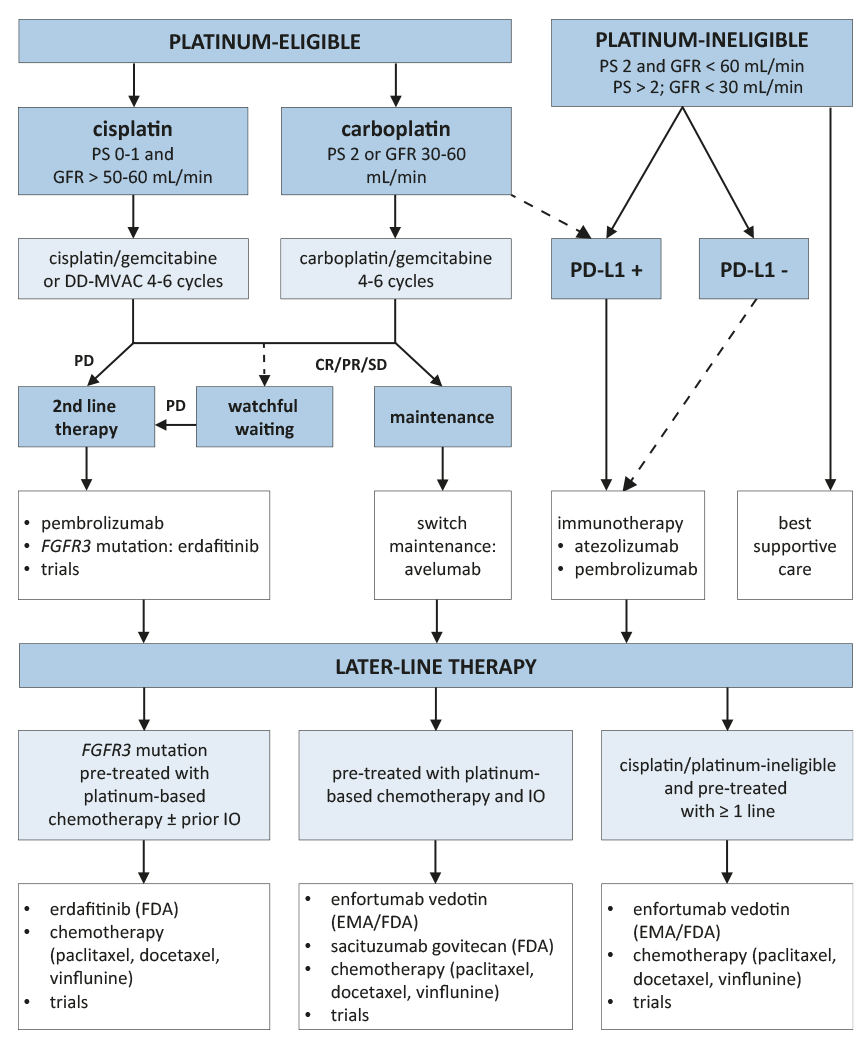
*Treatment within clinical trials is highly encouraged.
----- Dotted line: represents a treatment option which is not approved worldwide.
BSC = best supportive care; CR = complete response; DD-MVAC = dose dense methotrexate vinblastine doxorubicin cisplatin; EMA = European Medicines Agency; EV = enfortumab vedotin; FDA = US Food and Drug Administration; FGFR = fibroblast growth factor receptor; GFR = glomerular filtration rate; IO = immunotherapy; PR = partial response; PS = performance status; SD = stable disease.
7.8. Quality of life
7.8.1. Introduction
The evaluation of HRQoL considers physical, psychological, emotional and social functioning. In patients with MIBC, HRQoL is affected, particularly in the physical and social functioning domains [524,525].
Several questionnaires have been validated for assessing HRQoL in patients with BC, including FACT-G [526], EORTC QLQ-C30/BLM30 [527], SF-36 [528] and the Bladder Cancer Index (BCI) [529]. In spite of these validated questionnaires, there is heterogeneity in the measurements used to assess sexual health. A health questionnaire that covers the entire range of sexual health in bladder cancer patients is currently lacking [530].
Regardless of the which questionnaire is used, assessment of the baseline and post-treatment HRQoL is important. Questionnaires are helpful tools in clinical decision making, but, in addition, data support the prognostic value of baseline HRQoL [531].
7.8.2. Neoadjuvant chemotherapy
Two RCTs including patiens undergoing NAC have published their HRQoL data [441,532].
Huddart et al., analysed the subset of patients within the BC2001 trial who underwent NAC prior to (chemo)radiation. Using the FACT-BL questionnaire, no detrimental impact of NAC on HRQoL was observed [441]. Kitamura et al., reported on 64 patients included in the JCOG0209 study who underwent NAC (MVAC vs. MVAC and RC). An overall decline on HRQoL was reported directly following NAC using the FACT-BL questionnaire. However, no difference in HRQoL was observed after the consolidating RC.
7.8.3. Radical cystectomy and urinary diversion
Two systematic reviews and meta-analyses focused on HRQoL after RC and urinary diversion [356,533].
Yang et al., compared HRQoL of incontinent and continent urinary diversions (all types) including 29 studies (n = 3,754) of which 9 had a prospective design (one of which was randomised) [356]. Only three studies reported HRQoL data both pre- and post-operatively. All these three studies reported an initial deterioration in overall HRQoL but general health, functional and emotional domains at 12 months post-surgery were equal or better than baseline. Overall, no difference in HRQoL between continent and incontinent urinary diversion was reported although an ileal conduit may confer a small physical health benefit [533].
Cerruto et al., reported HRQoL comparing ileal conduit with orthotopic neobladder reconstruction [533]. A pooled analysis was performed including 18 studies (n = 1,553) of which the vast majority were retrospective studies. Although this study was hampered by methodological limitations, no statistical significant difference in overall HRQoL was found.
Altogether, there appears to be no superior type of urinary diversion in terms of overall HRQoL but it is rather a result of proper patient selection. An older and isolated patient is probably better served with an ileal conduit, whereas a younger patient with a higher level of interest in body image and sexuality is better off with an orthotopic diversion. The patient’s choice is the key to the selection of reconstruction method [356].
A number of RCTs comparing ORC with RARC (with either intra- or extracorporeal urinary diversion) have reported their HRQoL data [343,379,534,535]. All studies reported no statistical significant difference in HRQoL outcomes between surgical techniques.
7.8.4. Bladder-sparing trimodality therapy
The only HRQoL data in bladder sparing treatment collected in a RCT setting was published by Huddart et al. [441]. The primary endpoint was the change in the Bladder Cancer Subscale (BLCS), as part of the FACT-BL questionnaire, at one year post-treatment. Questionnaire return rate at one and five years was 70% and 60%, respectively. A reduction in HRQoL was seen in the majority of the domains immediately following RT, however, in most patients the HRQoL scores returned to baseline 6 months after RT and maintained at this level for five years. Approximately 33% of patients reported persistent lower Bladder Cancer Subscale scores after five years. Addition of chemotherapy did not affect the HRQoL outcomes.
7.8.5. Non-curative or metastatic bladder cancer
In non-curative or metastatic BC, HRQoL is reduced because of associated micturition problems, bleeding, pain and therefore disturbance of social and sexual life [536]. Beneficial impact of palliative surgery [537], RT [538], and/or chemotherapy on bladder-related symptoms have been described [539].
A HRQoL analysis was performed in platinum-refractory patients who were randomised to pembrolizumab vs. another line of chemotherapy (KEYNOTE-45 trial) [540]. It was reported that patients treated with pembrolizumab had stable or improved global health status/QoL, whereas those treated with investigators’ choice of chemotherapy experienced declines in global health [540].
Recently, HRQoL data was presented from cohort 1 of the EV-201 study including 125 patients treated with enfortumab vedotin after failing previous treatment with platinum chemotherapy and anti–PD-1/L1 therapy [541]. Patients who remained on enfortumab vedotin treatment showed no detoriation in HRQoL. In patients with bone metastases at baseline, pain control and possibly pain reduction was observed.
7.8.6. Summary of evidence and recommendations for health-related quality of life
Summary of evidence | LE |
Compared to non-cancer controls, the diagnosis and treatment of BC has a negative impact on HRQoL. | 2a |
There is no distinct difference in overall QoL between patients with continent or incontinent diversion. | 1b |
In patients with MIBC treated with RC, overall HRQoL declines immediately after treatment and recovers to baseline at 12 months post-operatively in most patients. | 1b |
In patients with MIBC treated with RT, overall HRQoL declines immediately after treatment, and recovers to baseline at 6 months post-treatment. | 1b |
HRQoL data are comparable for RARC (with either intracorporeal or extracorporeal urinary diversion) and ORC. | 1b |
In patients with MIBC treated with RT, concomitant chemotherapy or neo-adjuvant chemotherapy has no significant impact on HRQoL. | 1b |
In patients with platinum-refractory advanced UC, pembrolizumab may be superior in terms of HRQoL compared to another line of chemotherapy. | 1b |
Recommendations | Strength rating |
Use validated questionnaires to assess health-related quality of life in patients with muscle-invasive bladder cancer, both at baseline and post-treatment. | Strong |
Discuss the type of urinary diversion taking into account a patient preference, existing comorbidities, tumour variables and coping abilities. | Strong |