Why early detection for prostate cancer is vital
Prostate cancer kills one man every 45 minutes in the UK. Effective early detection is the key to reducing this mortality rate. Informing men about the risk of prostate cancer is crucial.
This article was written by Prof. Hein Van Poppel (BE) and Mrs. Sarah Collen (BE) of the European Association of Urology and by Ms. Sarah Coghlan (GB) and Ms. Kellie Paich (US) of Movember. It was published as part of the Men’s Health Campaign 2021 of Mediaplanet online via www.healthawareness.co.uk/mens-health/why-early-detection-for-prostate-cancer-is-vital/ and in a supplement inside The Guardian newspaper.
Prostate cancer is the most common cancer in men and the disease kills over 12,000 UK men every year. It is estimated that one in eight UK men will develop the disease at some point in their lives.
Caught in its early stages, prostate cancer can be cured and treated with more manageable side effects to patients. However, caught too late, it can have many serious effects on the lives of patients and their families. Treatment and care for advanced prostate cancer are also costly and place significant demands on the already hard-pressed NHS, with very little quality-of-life benefits for prostate cancer patients.
Effective early detection is a win-win
Around four in 10 prostate cancer cases are diagnosed at a late stage in England (2014) and Northern Ireland (2010-2014). In Scotland, this number is around six in 10 (2013-2014). One of the simplest ways of reducing the burdens on men, their families and the NHS would be to achieve a reduction in the proportion of men diagnosed with incurable advanced prostate cancer. Achieving effective early detection of prostate cancer is a win-win for patients and the NHS alike.
Unfortunately, this has been easier said than done. One of the main points of contention is that the UK’s National Screening Committee claims that the harms of prostate cancer screening still outweigh the benefits. This comes from a contentious issue around the use of prostate-specific antigen (PSA) testing. This blood test reveals if there is a heightened level of PSA in the blood, which can be a sign of prostate cancer.
The problem is that when PSA was first introduced, although it led to a decrease in mortality rates, it also led to overdiagnosis and overtreatment. Therefore, men who were at very low risk of developing lethal prostate cancer received intrusive biopsies or treatment that they potentially did not need.
We have come a long way from the initial issues of decades past. Clinicians and scientists in organisations like the European Association of Urology (EAU) and Movember have worked together in multi-disciplinary teams and found ways to piece together the jigsaw puzzle of early detection.
Men should be well informed
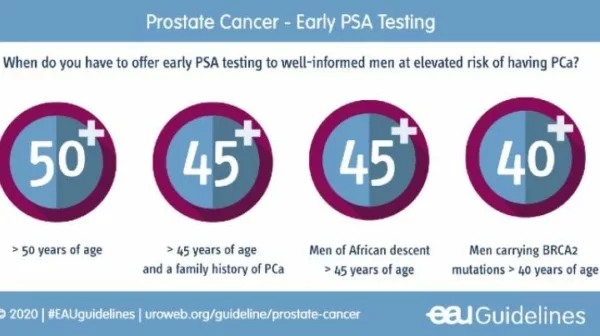
These clinicians and scientists work with the principle that men should be well informed about the availability and utility of PSA testing. Men should be aware that they are at an increased risk of developing prostate cancer as they increase in age, when they have a family history, have the BRCA gene mutation, and/or are of African descent (see the figure above).
Upon getting the PSA test result, clinicians can use widely available advanced risk calculators to decide if further tests are necessary. The introduction of new technology has brought about advances in non-invasive monitoring such as active surveillance, helping clinicians pursue the right treatment at the right time – if needed at all.
This demonstrates that new technology is turning the tide on early detection of prostate cancer. PSA testing does not need to cause over-diagnosis and over-treatment anymore – but instead results in more years lived with a high quality of life for patients and a reduction in prostate cancer mortality.