5. FOLLOW UP OF URINARY STONES
Patients suffering from urinary tract lithiasis have a predisposition to develop symptoms, complications, and recurrence of stones. Despite the rich literature published on urinary lithiasis very little has been written about how lithiasis patients should be monitored after their treatment.
There is no general agreement on whether and when stone patients should be released from their follow-up, nor when and how follow-up should occur for patients who need it. The main reason for this lack of agreement is the great clinical heterogeneity of stone disease among patients.
The EAU Urolithiasis Guidelines Panel performed a systematic review questioning the benefits and harms of scheduled follow-up for patients who underwent definitive treatment (extracorporeal shock wave lithotripsy, ureteroscopy, percutaneous nephrolithotripsy, medical chemoprophylaxis) for upper urinary tract stone disease [736].
The Panel aimed to answer three main questions regarding urolithiasis follow-up: a) In patients with no residual fragments, does imaging follow-up after treatment for upper urinary tract stones offer more clinical benefits than harms compared with no scheduled follow-up? b) In patients with residual fragments, does imaging follow-up after treatment for upper urinary tract stones offer more clinical benefits than harms compared with no scheduled follow-up? and c) Does biochemical urine analysis follow-up after treatment for upper urinary tract stones offer more clinical benefits than harms compared with no scheduled follow-up? There was a lack of comparative studies regarding follow-up versus no follow-up, so the primary endpoints were not reached. The panel used the data from the eligible observational and randomised studies included in the systematic review to identify the time of patient discharge after follow-up according to stone disease status (stone-free patients, patients with residual stones, patients with metabolic abnormalities), and to come to a consensus on frequency of follow-up and use of investigations.
From a pooled analysis of 5,467 stone-free patients, the Panel estimated that for a safety margin of 80%, patients should be followed-up using imaging, for at least two years (radiopaque stones), or at least three years (radiolucent stones) before discharge, while for a safety margin of 90% patients should be discharged after five years of no recurrence. Regarding residual disease, patients with fragments < 4mm could be offered either surveillance for up to four years, since intervention rates range between 17-29%, disease progression between 9-34% and spontaneous passage between 21-34% at 49 months. Patients with larger residual fragments should be offered further definitive intervention, since intervention rates are high (24-100%). Insufficient data exist for high-risk patients, but current literature dictates that patients who are adherent to targeted medical treatment seem to experience less stone growth or re-growth of residual fragments and may be discharged after 36-48 months of non-progressive disease on imaging (Figure 5.1).
A Panel consensus was reached after extensive discussion of data regarding frequency of follow-up. In stone-free general population, the vast majority of patients remained stone-free during the 1st year, in contrast with patients with metabolic abnormalities not under targeted medical treatment, < 40% were stone-free after three years of follow-up. Therefore, a more extensive follow-up is proposed for patients with metabolic abnormalities. Patients with small residual fragments < 4mm, showed a spontaneous expulsion at 17.9-46.5% and growth rate at 10.1-40.7% during the 1st year, while patients with larger fragments (> 4 mm) had only 9% of spontaneous expulsion at three years. Therefore, patients with small < 4mm, asymptomatic fragments should be followed-up or scheduled for an intervention according to patient preference, while those with larger stones should primarily be offered re-intervention. Proposed imaging consists of plain X-ray KUB and/or US, based on stone characteristics and clinicians’ preferences. Computed tomography scan should be reserved for symptomatic disease or pre-operative imaging, in order to avoid extensive radiation exposure (Figure 5.2) [736].
The information on stone composition can be used to counsel patients to set expectations and help plan the need for follow up and medical stone management [737].
Figure 5.1: Follow-up duration of Urinary stone patients after treatment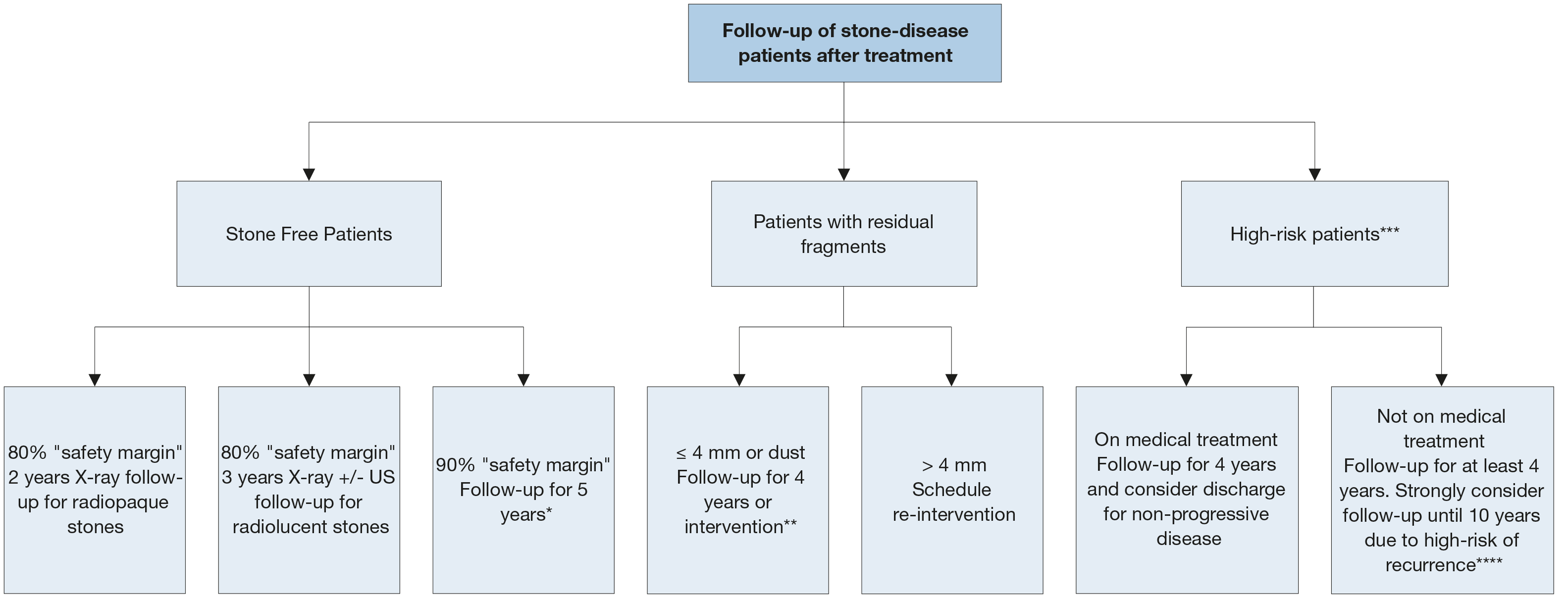 * Not enough data about subgroup analysis of radiolucent and radiopaque stones.
* Not enough data about subgroup analysis of radiolucent and radiopaque stones.
** According to patient preference or symptomatic disease.
*** Patients with diagnosed metabolic abnormalities.
**** Lifelong follow-up is advised but data are available up to 10 years.
Figure 5.2: Consensus on follow-up frequency and imaging modality to use after treatment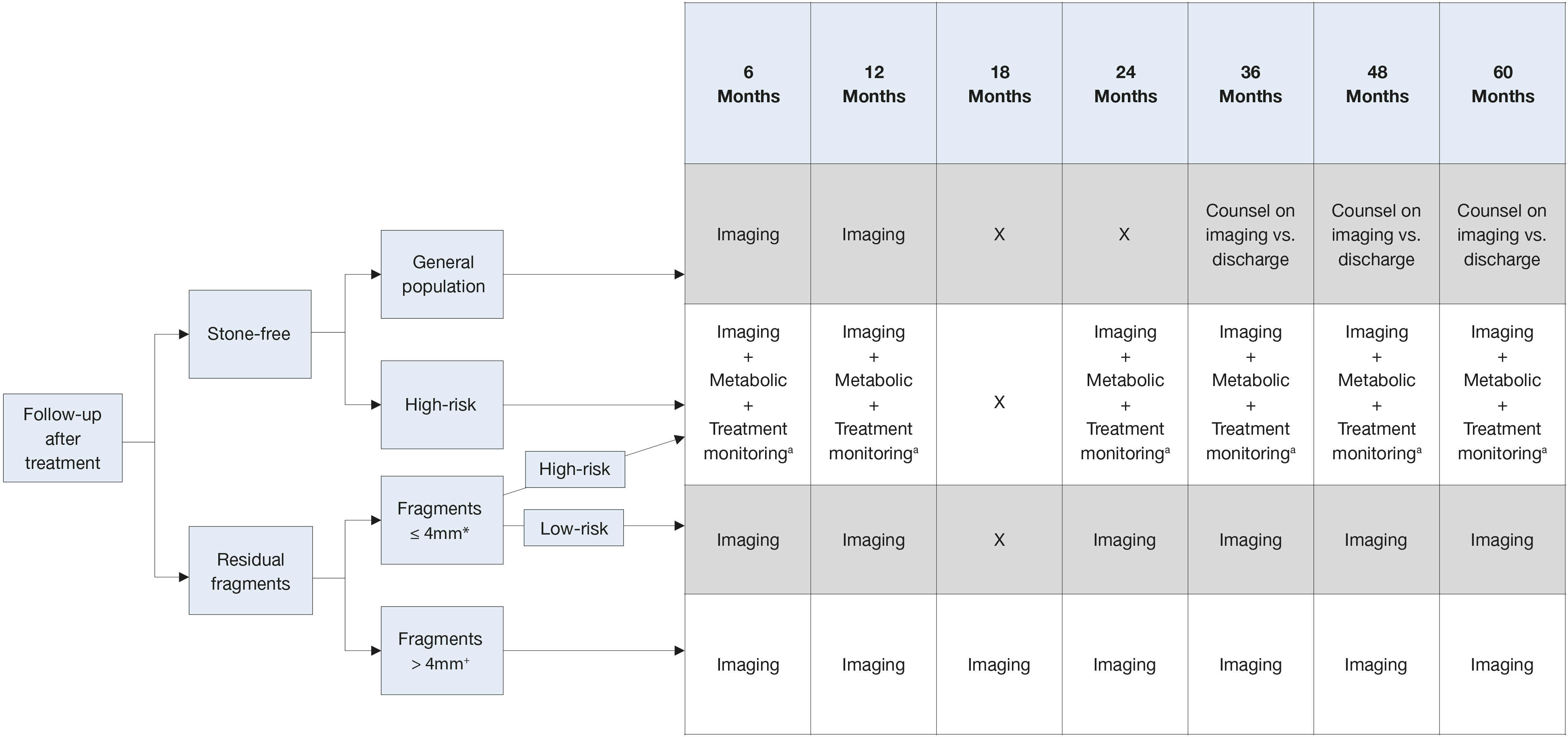 Stone free = No stone fragments on post-operative imaging (i.e. no stone fragments on CT/KUB/US).High-Risk = Known biochemical abnormality (i.e,: hypercalciuria, hypocitraturia, hyperuricosuria, RTA or high-risk stone type such as struvite). Imaging = plain film KUB &/or kidney ultrasonography (KUS) based on clinicians’ preference and stone characteristics. Consider CT if patient is symptomatic or if intervention is planned.
Stone free = No stone fragments on post-operative imaging (i.e. no stone fragments on CT/KUB/US).High-Risk = Known biochemical abnormality (i.e,: hypercalciuria, hypocitraturia, hyperuricosuria, RTA or high-risk stone type such as struvite). Imaging = plain film KUB &/or kidney ultrasonography (KUS) based on clinicians’ preference and stone characteristics. Consider CT if patient is symptomatic or if intervention is planned.
* Clinicians may choose the imaging-only pathway in patients with fragments < 2 mm.
o Treatment monitoring for side effects, intolerance, and compliance.
+ Panel recommends reintervention however close follow up may be considered for some patients at high risk for reintervention based on clinicians’ preference.