3. GUIDELINES
3.1. Prevalence, aetiology, risk of recurrence
3.1.1. Introduction
Stone incidence depends on geographical, climatic, ethnic, dietary, and genetic factors. The recurrence risk is basically determined by the disease or disorder causing the stone formation. Accordingly, the prevalence rates for urinary stones vary from 1% to 20% [9]. In countries with a high standard of life such as Sweden, Canada or the USA, renal stone prevalence is notably high (> 10%). For some areas, an increase of more than 37% over the last 20 years has been reported [10-12]. There is emerging evidence linking nephrolithiasis to the risk of chronic Kidney disease (CKD) [13].
Stones can be stratified into those caused by: infections, non-infectious causes, genetic defects [14]; or adverse drug effects (drug stones) (Table 3.1). See also section 3.2.
Table 3.1: Stones classified by aetiology
Non-infection stones | ||
• Calcium oxalate | • Calcium phosphate | • Uric acid • Ammonium urate* |
Infection stones | ||
• Magnesium ammonium phosphate | • Highly carbonated apatite | • Ammonium urate |
Genetic causes | ||
• Cystine | • Xanthine | • 2,8-Dihydroxyadenine |
Drug stones |
*In children in developing countries; in patients with anorexia or laxative-abuse.
3.1.2. Stone composition
Stone composition is the basis for further diagnostic and management decisions. Stones are often formed from a mixture of substances. Table 3.2 lists the most clinically relevant substances and their mineral components.
Table 3.2: Stone composition
Chemical name | Mineral name [15] | Chemical formula |
Calcium oxalate monohydrate | Whewellite | CaC2O4.H2O |
Calcium oxalate dihydrate | Weddelite | CaC2O4.2H2O |
Basic calcium phosphate | Apatite | Ca10(PO4)6.(OH)2 |
Calcium hydroxyl phosphate | Carbonate apatite | Ca5(PO4)3(OH) |
b-tricalcium phosphate | Whitlockite | Ca3(PO4)2 |
Carbonate apatite phosphate | Dahllite | Ca5(PO4)3OH |
Calcium hydrogen phosphate dihydrate | Brushite | CaHPO4.2H2O |
Calcium carbonate | Aragonite | CaCO3 |
Octacalcium phosphate | - | Ca8H2(PO4)6.5H2O |
Uric acid | Uricite | C5H4N4O3 |
Uric acid dihydrate | Uricite | C5H4O3.2H20 |
Ammonium urate | - | NH4C5H3N4O3 |
Sodium acid urate monohydrate | - | NaC5H3N4O3.H2O |
Magnesium ammonium phosphate hexahydrate | Struvite | MgNH4PO4.6H2O |
Magnesium acid phosphate trihydrate | Newberyite | - |
Magnesium ammonium phosphate monohydrate | Dittmarite | - |
Cystine | - | - |
Xanthine | - | - |
2,8-Dihydroxyadenine | - | - |
Proteins | - | - |
Cholesterol | - | - |
Calcite | - | - |
Potassium urate | - | - |
Trimagnesium phosphate | - | - |
Melamine | - | - |
Matrix | - | - |
Drug stones | Active compounds crystallising in urine | - |
Foreign body calculi | - | - |
3.1.3. Risk groups for stone formation
The risk status of stone formers should be determined in a holistic way taking into consideration not only the probability of stone recurrence or regrowth, but also the risk of CKD and mineral and bone disorder (MBD) [16,17], and is imperative for pharmacological treatment. About 50% of recurrent stone formers have just one lifetime recurrence [11,18]. A recent review of first-time stone formers calculated a recurrence rate of 26% in five years’ time [19]. Highly recurrent disease is observed in slightly more than 10% of patients. Stone type and disease severity determine low- or high-risk stone formers (Table 3.3) [20,21].
Table 3.3: High-risk stone formers [20-36]
General factors |
Early onset of urolithiasis (especially children and teenagers) |
Familial stone formation |
Recurrent stone formers |
Short time since last stone episode |
Brushite-containing stones (CaHPO4.2H2O) |
Uric acid and urate-containing stones |
Infection stones |
Solitary kidney (the kidney itself does not particularly increase the risk of stone formation, but prevention of stone recurrence is of crucial importance to avoid acute renal failure) |
Chronic Kidney Disease (CKD) |
Diseases associated with stone formation |
Hyperparathyroidism |
Metabolic syndrome |
Mineral Bone Disorder (MBD) |
Nephrocalcinosis |
Polycystic kidney disease (PKD) |
Gastrointestinal diseases (i.e., jejuno-ileal bypass, intestinal resection, Crohn’s disease, malabsorptive conditions, enteric hyperoxaluria after urinary diversion, exocrine pancreatic insufficiency) and bariatric surgery |
Increased levels of vitamin D |
Sarcoidosis |
Spinal cord injury, neurogenic bladder |
Genetically determined stone formation |
Cystinuria (type A, B and AB) |
Primary hyperoxaluria (PH) |
Renal tubular acidosis (RTA) type I |
2,8-Dihydroxyadeninuria |
Xanthinuria |
Lesch-Nyhan syndrome |
Cystic fibrosis |
Drug-induced stone formation (see Table 4.11) |
Anatomical abnormalities associated with stone formation |
Medullary sponge kidney (tubular ectasia) |
Ureteropelvic junction (UPJ) obstruction |
Calyceal diverticulum, calyceal cyst |
Ureteral stricture |
Vesico-uretero-renal reflux |
Horseshoe kidney |
Ureterocele |
Environmental and professional factors |
High ambient temperatures |
Chronic lead and cadmium exposure |
A comprehensive evaluation of stone risk in patients should also include the risk of developing CKD, end-stage kidney disease (ESKD), and MBD (Tables 3.4, 3.5 and 3.6) [16]. Urolithiasis can compromise renal function because of the renal stone (obstruction, infection), renal tissue damage due to the primary condition causing stone formation (some genetic diseases, nephrocalcinosis, enteric hyperoxaluria, etc.), or urological treatments for the condition [16]. Certain risk factors have been shown to be associated with such a risk in stone formers, as shown below.
Table 3.4 Risk factors for CKD and ESKD in stone formers
Risk factors for CKD/ESKD in stone formers |
Female gender |
Overweight |
Frequent urinary tract infection (UTI) |
Struvite stones |
Acquired single kidney |
Neurogenic bladder |
Previous obstructive nephropathy |
Ileal conduit |
Furthermore, some specific kinds of urolithiasis also carry a particular risk of developing CKD/ESKD as shown below.
Table 3.5 Risk factors for CKD and renal stones
Risk of chronic kidney disease and renal stones |
Possible risk of CKD |
Xanthine stones |
Indinavir stones |
Distal renal tubular acidosis (incomplete) |
Primary hyperparathyroidism |
Eating disorders and laxative abuse |
Medullary sponge kidney |
Moderate risk of CKD |
Brushite stones |
2,8-Dihydroxyadenine stones |
Sarcoidosis |
Pyelo-ureteral or ureteral strictures |
High risk of CKD |
Cystine stones |
Struvite stones |
Stones in a single kidney |
Distal renal tubular acidosis (complete) |
Secondary hyperoxaluria (bariatric surgery, inflammatory bowel disease, bowel resection and malabsorptive syndromes) |
Other forms of nephrocalcinosis (often associated with genetic conditions with hypercalciuria) |
Anatomical abnormalities of the kidney and urinary tract (for example, horseshoe kidney, ureterocele and vesicoureteral reflux) |
Neurological bladder |
Very high risk of CKD |
Primary hyperoxaluria |
Autosomal dominant polycystic kidney |
Table 3.6 Risk factors for metabolic bone disease and calcium renal stones
Risk of metabolic bone disease and calcium renal stones |
Distal renal tubular acidosis (complete or incomplete) |
Medullary sponge kidney |
Primary hyperparathyroidism |
Malabsorptive syndromes |
Fasting hypercalciuria |
Genetic disorders |
3.2. Classification of stones
Urinary stones can be classified according to size, location, X-ray characteristics, aetiology of formation, composition, and risk of recurrence [11,37,38].
3.2.1. Stone size
Stone size is usually given in one or two dimensions, and stratified into those measuring up to 5, 5-10, 10-20, and > 20 mm in largest diameter.
3.2.2. Stone location
Stones can be classified according to anatomical position: upper, middle, or lower calyx; renal pelvis; upper, middle, or distal ureter; and urinary bladder.
3.2.3. X-ray characteristics
Stones can be classified according to plain X-ray appearance [kidney-ureter-bladder (KUB) radiography] (Table 3.6), which varies according to mineral composition [38]. Non-contrast-enhanced computed tomography (NCCT) can be used to classify stones according to density, inner structure, and composition, which can affect treatment decisions (Section 3.3) [37,38].
Table 3.7: X-ray characteristics
Radiopaque | Poor radiopacity | Radiolucent |
Calcium oxalate dehydrate | Magnesium ammonium phosphate | Uric acid |
Calcium oxalate monohydrate | Apatite | Ammonium urate |
Calcium phosphates | Cystine | Xanthine |
2,8-Dihydroxyadenine | ||
Drug-stones (Section 4.11) |
3.3. Diagnostic evaluation
3.3.1. Diagnostic imaging
The most appropriate imaging modality will be determined by the clinical situation, which will differ depending on if a ureteral or a renal stone is suspected.
Standard evaluation includes a detailed medical history and physical examination. Patients with ureteral stones usually present with loin pain, vomiting, and sometimes fever, but may also be asymptomatic [39]. Immediate evaluation is indicated in patients with solitary kidney, fever or when there is doubt regarding a diagnosis of renal colic. Ultrasound (US) should be used as the primary diagnostic imaging tool, although pain relief, or any other emergency measures, should not be delayed by imaging assessments. Ultrasound is safe (no risk of radiation), reproducible and inexpensive. It can identify stones located in the calyces, pelvis, and pyeloureteric and vesico-ureteral junctions (US with filled bladder), as well as in patients with upper urinary tract (UUT) dilatation. Ultrasound has a sensitivity of 45% and specificity of 94% for ureteral stones and a sensitivity of 45% and specificity of 88% for renal stones [40,41].
The sensitivity and specificity of KUB is 44-77% [42]. Kidney-ureter-bladder radiography should not be performed if NCCT is being considered [43]; however, it is helpful in differentiating between radiolucent and radiopaque stones and should be used for comparison during follow-up.
3.3.1.1. Evaluation of patients with acute flank pain/suspected ureteral stones
Non-contrast-enhanced computed tomography (CT) has become the standard for diagnosing acute flank pain and has replaced intravenous urography (IVU). Non-contrast-enhanced CT can determine stone diameter and density. When stones are absent, the cause of abdominal pain should be identified. In evaluating patients with suspected acute urolithiasis, NCCT is significantly more accurate than IVU or US [44].
Non-contrast-enhanced CT can detect uric acid and xanthine stones, which are radiolucent on plain films, but not indinavir stones [45]. Non-contrast-enhanced CT can determine stone density, inner structure of the stone, skin-to-stone distance, and surrounding anatomy; all of which affect selection of treatment modality [38,46-48]. The advantage of non-contrast imaging must be balanced against loss of information on renal function and urinary collecting system anatomy, as well as higher radiation dose [49-52].
Radiation risk can be reduced by low-dose CT, which may, however, be difficult to introduce in standard clinical practice [53-57]. In patients with a body mass index (BMI) < 30, low-dose CT has been shown to have a sensitivity of 86% for detecting ureteral stones < 3 mm and 100% for calculi > 3 mm [58]. A meta-analysis (MA) of prospective studies [55] has shown that low-dose CT diagnosed urolithiasis with a pooled sensitivity of 93.1% (95% confidence interval [CI]: 91.5-94.4), and a specificity of 96.6% (95% CI: 95.1-97.7%). Dual-energy CT can differentiate uric acid containing stones from calcium-containing stones [59,60].
Summary of evidence | LE |
Non-contrast-enhanced CT is used to confirm stone diagnosis in patients with acute flank pain, as it is superior to IVU. | 1a |
Enhanced CT enables 3D reconstruction of the collecting system, as well as measurement of stone density and skin-to-stone distance. | 2a |
Recommendations | Strength rating |
Immediate imaging is indicated with fever or solitary kidney, and when diagnosis is doubtful. | Strong |
Use non-contrast-enhanced computed tomography to confirm stone diagnosis in patients with acute flank pain following initial ultrasound assessment. | Strong |
Perform a contrast study if stone removal is planned and the anatomy of the renal collecting system needs to be assessed. | Strong |
3.3.2. Diagnostics - metabolism-related
Besides imaging, each emergency patient with urolithiasis needs a succinct biochemical work-up of urine and blood test. At this point, no distinction is made between high- and low-risk patients for stone formation.
3.3.2.1. Basic laboratory analysis - non-emergency urolithiasis patients
Biochemical work-up is similar for all stone patients. However, if no intervention is planned, examination of sodium, potassium, C-reactive protein (CRP), and blood coagulation time can be omitted. Only patients at high risk for stone recurrence should undergo a more specific analytical programme [21]. Stone-specific metabolic evaluation is described in Chapter 4.
The easiest method for diagnosing stones is by analysis of a passed stone using a validated method as listed in section 3.3.2.3. Once the mineral composition is known, a potential metabolic disorder can be identified.
3.3.2.2. Analysis of stone composition
Stone analysis should be performed in all first-time stone formers.
In clinical practice, repeat stone analysis is needed in the case of:
- recurrence under pharmacological prevention;
- early recurrence after interventional therapy with complete stone clearance;
- late recurrence after a prolonged stone-free period [61,62].
Patients should be instructed to filter their urine to retrieve a concrement for analysis. Stone passage and restoration of normal renal function should be confirmed.
The preferred analytical procedures are infrared spectroscopy (IRS) or X-ray diffraction (XRD) [63-65]. Equivalent results can be obtained by polarisation microscopy. Chemical analysis (wet chemistry) is generally deemed to be obsolete [63,66].
3.3.2.3. Recommendations for laboratory examinations and stone analysis 21, 27, 67-69]
Recommendations | Strength rating |
Urine | |
Dipstick test of spot urine sample: • red cells; • white cells; • nitrites; • approximate urine pH; • urine microscopy and/or culture. | Weak |
Blood | |
Serum blood sample: • creatinine; • uric acid; • (ionised) calcium; • sodium; • potassium; • blood cell count; • C-reactive protein. | Strong |
Perform a coagulation test (partial thromboplastin time and international normalised ratio) if intervention is likely or planned. | Strong |
Perform stone analysis in first-time formers using a valid procedure (X-ray diffraction or infrared spectroscopy). | Strong |
Repeat stone analysis in patients presenting with: • recurrent stones despite drug therapy; • early recurrence after complete stone clearance; • late recurrence after a long stone-free period because stone composition may change. | Strong |
3.3.3. Diagnosis in special groups and conditions
3.3.3.1. Diagnostic imaging during pregnancy
In pregnant women radiation exposure may cause non-stochastic (teratogenesis) or stochastic (carcinogenesis/mutagenesis) effects. Teratogenic effects are cumulative with increasing dose and require a threshold dose (< 50 mGy are considered as safe) and depend on the gestation age (minimum risk prior to 8th week and after the 23rd week). Carcinogenesis (doses even < 10 mGy present a risk) and mutagenesis (500-1000 mGy doses are required, far in excess of the doses in common radiographic studies) get worse with increasing dose but they do not require a dose threshold and are not dependent on gestational age [70].
There is no imaging modality that should be routinely repeated in pregnant women. Scientific societies and organisations agree on the safety of diagnostic evaluation when US [71], X-ray imaging [72,73], and MRI [74,75] are used as and when indicated [76-82]. A radiographic procedure should not be withheld from a pregnant woman if the procedure is clearly indicated and doing so will affect her medical care.
It is generally recommended that an investigation resulting in an absorbed dose to the foetus of greater than 0.5 mGy requires justification.
Ultrasound (when necessary, using changes in renal resistive index and transvaginal/transabdominal US with a full bladder) has become the primary radiological diagnostic tool when evaluating pregnant patients suspected of renal colic. However, normal physiological changes in pregnancy can mimic ureteral obstruction [78-80].
Magnetic resonance imaging can be used, as a second-line option [76], to define the level of urinary tract obstruction, and to visualise stones as a filling defect [74]. As 3 Tesla (T) MRI has not been evaluated in pregnancy, the use of 1.5T is currently recommended [77,82]. The use of gadolinium is not routinely recommended in pregnancy to avoid toxic effects to the embryo [78].
For the detection of urolithiasis during pregnancy, low-dose CT is associated with a higher positive predictive value (95.8%), compared to MRI (80%) and US (77%). As per White et al., low-dose CT offers improved diagnostic accuracy that can avoid negative interventions such as ureteroscopy [83]. Although low-dose CT protocols reduce the radiation exposure, judicious use is currently recommended in pregnant women as a last-line option [78].
Summary of evidence | LE |
Only low-level data exist for imaging in pregnant women supporting US and MRI. | 3 |
Recommendations | Strength rating |
Use ultrasound as the preferred method of imaging in pregnant women. | Strong |
Use magnetic resonance imaging as a second-line imaging modality in pregnant women. | Strong |
Use low-dose computed tomography as a last-line option in pregnant women. | Strong |
3.3.3.2. Diagnostic imaging in children
Children with urinary stones have a high risk of recurrence; therefore, standard diagnostic procedures for high-risk patients apply, including a valid stone analysis (Section 3.1.3 and Chapter 4). The most common nonmetabolic disorders facilitating stone formation are vesico-ureteral reflux (VUR), UPJ obstruction, neurogenic bladder, and other voiding difficulties [84].
When selecting diagnostic procedures to identify urolithiasis in children, it should be remembered that these patients might be uncooperative, require anaesthesia, and may be sensitive to ionising radiation. Again, the principle of ALARA (As Low As Reasonably Achievable) should be observed [85-87].
Ultrasound
Ultrasound is the primary imaging technique [88] in children. Its advantages are absence of radiation and no need for anaesthesia. Imaging should include both the fluid-filled bladder with adjoining portion of the ureters, as well as the upper ureter [89-93]. Colour Doppler US shows differences in the ureteral jet [90] and resistive index of the arciform arteries of both kidneys, which are indicative of the grade of obstruction [91]. Nevertheless, US fails to identify stones in > 40% of children [92-95] and provides limited information on renal function.
Plain films (KUB radiography)
Kidney-ureter-bladder radiography can help to identify stones and their radiopacity and facilitate follow-up.
Intravenous urography
The radiation dose for IVU is comparable to that for voiding cysto-urethrography (0.33 mSV) [96]. However, the need for contrast medium injection is a major drawback.
Non-contrast-enhanced computed tomography
Recent low-dose CT protocols have been shown to significantly reduce radiation exposure [52,97,98]. In children, only 5% of stones escape detection by NCCT [90,98,99]. Sedation or anaesthesia is rarely needed with modern high-speed CT equipment.
Magnetic resonance urography
Magnetic resonance urography (MRU) cannot be used to detect urinary stones. However, it might provide detailed anatomical information about the urinary collecting system, the location of an obstruction or stenosis in the ureter, and renal parenchymal morphology [100].
3.3.3.2.1. Summary of evidence and recommendations for diagnostic imaging in children
Summary of evidence | LE |
Ultrasound is the first-line imaging modality in children when a stone is suspected; it should include the kidney, fluid-filled bladder, and the ureter next to the kidney and the (filled) bladder. | 2b |
A kidney-ureter-bladder radiography (or low-dose NCCT) is an alternative investigation if US will not provide the required information. | 2b |
Recommendations | Strength rating |
Complete a metabolic evaluation based on stone analysis in all children. | Strong |
Collect stone material for analysis to classify the stone type. | Strong |
Perform ultrasound as first-line imaging modality in children when a stone is suspected; it should include the kidney, fluid-filled bladder, and the ureter. | Strong |
Perform a kidney-ureter-bladder radiography (or low-dose non-contrast-enhanced computed tomography) if ultrasound will not provide the required information. | Strong |
3.4. Disease Management
The treatment of urolithiasis is based on many parameters and is individualised for each patient. Parameters such as the size, number, location, and constitution of the stones are cornerstones for deciding the treatment. In addition, the morphology, shape, volume, mobility, and hardness of the stone should be considered. Finally, the anatomy and compliance of the entire pelvic-calyceal system should be assessed for each patient. The design of therapeutic algorithms including all of the above parameters is difficult mainly due to the great diversity of lithiasis disease per patient. Furthermore, there is a significant lack of comparative clinical studies to support development of algorithms using parameters other than stone size and composition.
3.4.1. Renal colic
Pain relief
Non-steroidal anti-inflammatory drugs (NSAIDs) (including metamizoledipyrone), and paracetamol are effective in patients with acute stone colic [101], and have better analgesic efficacy than opioids [102]. Ibuprofen compared to ketorolac is a more rapid acting drug in controlling pain caused by renal colic with a similar side effect profile [103].
Pain relief from intramuscular (i.m.) diclofenac compared favourably with those from intravenous (i.v.) ibuprofen and i.v. ketorolac; however, no recommendation can be given due to the way in which the results have been reported [104]. The addition of antispasmodics to NSAIDs does not result in better pain control. Patients receiving NSAIDs are less likely to require further analgesia in the short term. It should be taken into consideration that the use of diclofenac and ibuprofen increased major coronary events [101,102]. Diclofenac is contraindicated in patients with congestive heart failure (New York Heart Association class II-IV), ischaemic heart disease and peripheral arterial- and cerebrovascular disease. Patients with significant risk factors for cardiovascular events should be treated with diclofenac only after careful consideration. As risks increase with dose and duration, the lowest effective dose should be used for the shortest duration [105,106].
In a RCT including 150 patients, Intradermal sterile water injection (ISWI) and diclofenac (i.m.) were shown equally effective for pain relief in acute renal colic. Intradermal sterile water injection may be an alternative to NSAIDs in pregnant patients or others where NSAIDs are contra-indicated [107].
Opioids, particularly pethidine, are associated with a high rate of vomiting compared to NSAIDs and carry a greater likelihood of further analgesia being needed [101,108] (see below). If an opioid is used, it is recommended that it is not pethidine. Combination of opioids and NSAIDs increase analgetic effect compare to opioids alone [109]. Data on other types of non-opioid and non-NSAID medication is increasing. Ketamine in combination with morphine, compared to morphine alone, leads to morphine consumption reduction, less pain, nausea and vomiting [110-112]. Patients receiving ketamine and NSAIDs attained greater reduction in pain scores with less side effects, and better functional state, as well as less further analgesia requirement than those administered pethidine [113]. However, when comparing ketamine vs. NSAID (ketorolac) alone, equal efficacy but higher rates of dizziness, agitation and hypertension with ketamine were observed [114]. Conflicting results have been reported regarding the utility of intravenous lidocaine. Acupuncture seems to be effective in renal colic alone or in combination, but there is limited data [115,116].
Prevention of recurrent renal colic
Facilitation of passage of ureteral stones is discussed in Section 3.4.9. For patients with ureteral stones that are expected to pass spontaneously, NSAID tablets or suppositories (e.g., diclofenac sodium, 100-150 mg/day, 3-10 days) may help reduce inflammation and the risk of recurrent pain [117,118]. Although diclofenac can affect renal function in patients with already reduced function, it has no functional effect in patients with normal renal function [119].
The systematic review and MA by Hollingsworth et al., [120] addressed pain reduction as a secondary outcome and concluded that medical expulsive therapy (MET) seems efficacious in reducing pain episodes of patients with ureteral stones.
If analgesia cannot be achieved medically, drainage, using stenting, percutaneous nephrostomy, or stone removal, is indicated [121].
3.4.1.1. Summary of evidence and recommendations for the management of renal colic
Summary of evidence | LE |
Non-steroidal anti-inflammatory drugs are very effective in treating renal colic and are superior to opioids. | 1b |
For symptomatic ureteral stones, stone removal as first-line treatment is a feasible option in selected patients. | 1b |
Recommendations | Strength rating |
Offer a non-steroidal anti-inflammatory as the first drug of choice; e.g., metamizole* (dipyrone); alternatively paracetamol or, depending on cardiovascular risk factors, diclofenac**, indomethacin or ibuprofen***. | Strong |
Offer opioids (hydromorphine, pentazocine or tramadol) as a second choice. | Weak |
Offer renal decompression or ureteroscopic stone removal in case of analgesic refractory colic pain. | Strong |
* Maximum single oral dose recommended 1000 mg, total daily dose up to 5000 mg, not recommended in the last three months of pregnancy 122. ** Affects glomerular filtration rate (GFR) in patients with reduced renal function.*** Recommended to counteract recurrent pain after ureteral colic.
3.4.2. Management of sepsis and/or anuria in obstructed kidney
The obstructed kidney with all signs of urinary tract infection (UTI) and/or anuria is a urological emergency. Urgent decompression is often necessary to prevent further complications in infected hydronephrosis secondary to stone-induced, unilateral or bilateral, renal obstruction.
Decompression
Currently, there are two options for urgent decompression of obstructed collecting systems [123]:
- placement of an indwelling ureteral stent;
- percutaneous placement of a nephrostomy tube.
There is little evidence to support the superiority of percutaneous nephrostomy over retrograde stenting for primary treatment of infected hydronephrosis. There is no good quality evidence to suggest that ureteral stenting has more complications than percutaneous nephrostomy [124,125].
Only one RCT [126] compared different modalities of decompression of acute infected hydronephrosis. Two other small RCTs compared stenting vs. nephrostomy tube placement in patients with acute kidney injury and demonstrated both to be effective in decompressing the collecting system [127,128]. The complications of percutaneous nephrostomy insertion have been reported consistently, but those of ureteral stent insertion are less well described [124]. Definitive stone removal should be delayed until the infection is cleared following a complete course of antimicrobial therapy. A small RCT showed the feasibility of immediate ureteroscopic stone removal combined with an appropriate antibiotic regimen; however, at the cost of longer hospital stay and higher analgesic requirements [129].
Further measures
Following urgent decompression of the obstructed and infected urinary collecting system, both urine- and blood samples should be sent for culture-antibiogram sensitivity testing and antibiotics should be initiated immediately thereafter or continued, if initiated prior to testing. The regimen should be re-evaluated in the light of the culture-antibiogram results. Although clinically well accepted, the impact of a second antibiogram test on treatment outcome has not yet been evaluated. Intensive care might become necessary [130].
3.4.2.1. Summary of evidence and recommendations for the management of sepsis and anuria
Summary of evidence | LE |
For decompression of the renal collecting system, ureteral stents and percutaneous nephrostomy catheters are equally effective. | 1b |
Recommendations | Strength rating |
Urgently decompress the collecting system in case of sepsis with obstructing stones, using percutaneous drainage or ureteral stenting. | Strong |
Delay definitive treatment of the stone until sepsis is resolved. | Strong |
Collect (again) urine for antibiogram test following decompression. | Strong |
Start antibiotics immediately (+ intensive care, if necessary). | Strong |
Re-evaluate antibiotic regimen following antibiogram findings. | Strong |
3.4.3. Medical expulsive therapy
Several drug classes including α-blockers, calcium channel inhibitors and phosphodiesterase type 5 inhibitors (PDEI-5) are used for MET [131-134]. A class effect of α-blockers in MET has been demonstrated in MAs although this is an off-label indication [135-137]. However, there is contradictory evidence between these studies and several well-designed, multicentre, placebo-controlled, double-blinded randomised studies showing limited, or no, benefit using α-blockers, besides some advantage for distal ureteral stones > 5 mm [138-142]. Based on studies with a limited number of patients [134,135,143,144], no recommendation for the use of PDEI-5 or corticosteroids in combination with α-blockers in MET can be made. The panel concludes that MET using α-blockers seems efficacious in the treatment of patients with distal ureteral stones > 5 mm who are amenable to conservative management. Medical expulsive therapy in special situations is addressed in the relevant chapters.
3.4.3.1. Summary of evidence and recommendations for MET
Summary of evidence | LE |
Medical expulsive therapy seems to be efficacious for treating patients with ureteral stones who are amenable to conservative management. The greatest benefit might be among those with > 5 mm (distal) ureteral stones. | 1a |
Insufficient data exist to support the use of PDEI-5 or corticosteroids in combination with α-blockers as an accelerating adjunct. | 2a |
Alpha-blockers increase stone expulsion rates in distal ureteral stones > 5 mm. | 1a |
A class effect of α-blockers has been demonstrated. | 1a |
Recommendation | Strength rating |
Consider α-blockers as medical expulsive therapy as one of the treatment options for (distal) ureteral stones > 5 mm. | Strong |
3.4.4. Chemolysis
Percutaneous irrigation chemolysis
Percutaneous chemolysis is rarely used nowadays, for practical reasons. Percutaneous irrigation chemolysis may be an option for infection-stones and theoretically also for uric acid stones. For dissolution of struvite stones, Suby’s G solution (10% hemiacidrin; pH 3.5-4) can be used. The method has been described in case series and literature reviews [145-147].
Oral chemolysis
Stones composed of uric acid, but not sodium or ammonium urate stones, can be dissolved by oral chemolysis. Prior stone analysis may provide information on stone composition. Urinary pH measurement and X-ray characteristics can provide information on the type of stone.
Oral chemolitholysis is based on alkalinisation of urine by application of alkaline citrate or sodium bicarbonate. The pH should be adjusted to 7.0-7.2. Chemolysis is more effective at a higher pH, which might, however, promote calcium phosphate stone formation. Patients will need to adjust the dosage of alkalising medication by self-monitoring the pH of their urine. No RCTs are available for this therapy, which has been in use for decades. Rodman, et al., [148] reviewed the principles and provided guidance to its clinical use, which was supported by Becker, et al., in 2007 [149] and Elsawy et al. in 2019 [150]. Monitoring of radiolucent stones during therapy is the domain of US; however, repeat-NCCT might be necessary [148,149].
In the case of uric acid obstruction of the collecting system, oral chemolysis in combination with urinary drainage is indicated [151]. A combination of alkalinisation with tamsulosin can increase the frequency of spontaneous passage of distal ureteral uric acid stones as shown in one RCT for stones > 5 mm [151]. Additional shock wave lithotripsy (SWL) might help to improve the results but evidence is weak [152].
3.4.4.1. Summary of evidence and recommendations for chemolysis
Summary of evidence | LE |
Irrigation chemolysis has been used in limited clinical settings to dissolve struvite stones. | 3 |
Uric acid stones > 5mm can be dissolved based on oral alkalinisation of the urine above 7.0. | 3 |
For obstructing uric acid stones, a combination of oral chemolysis with tamsulosin is more effective than each substance alone, particularly in stones > 8 mm. | 1b |
Recommendations (oral chemolysis of uric acid stones) | Strength rating |
Inform the patient how to monitor urine-pH by dipstick and to modify the dosage of alkalising medication according to urine pH, as changes in urine pH are a direct consequence of such medication. | Strong |
Carefully monitor patients during/after oral chemolysis of uric acid stones. | Strong |
Combine oral chemolysis with tamsulosin in case of (larger) ureteral stones (if active intervention is not indicated). | Weak |
3.4.5. Extracorporeal shock wave lithotripsy (ESWL)
The success of SWL depends on the efficacy of the lithotripter and the following factors:
- size, location (ureteral, pelvic or calyceal), and composition (hardness) of the stones (Section 3.4.9.3);
- patient’s habitus (Section 3.4.10.3);
- performance of SWL (best practice, see below).
Each of these factors significantly influences the retreatment rate and final outcome of SWL.
Best clinical practiceStenting
Routine use of internal stents before SWL does not improve stone free rates (SFRs), nor lowers the number of auxiliary treatments. It may, however, reduce formation of steinstrasse [153-156].
Pacemaker
Patients with a pacemaker can be treated with SWL, provided that appropriate technical precautions are taken. Patients with implanted cardioverter defibrillators must be managed with special care (firing mode temporarily reprogrammed during SWL treatment). However, this might not be necessary with new-generation lithotripters [157].
Shock wave rate
Lowering shock wave frequency from 120 to 60-90 shock waves/min improves SFRs [158-166]. Ultraslow frequency 30 shock waves/min may increase SFR [167]. Tissue damage increases with shock wave frequency [168-171].
Number of shock waves, energy setting and repeat treatment sessions
The number of shock waves that can be delivered at each session depends on the type of lithotripter and shock wave power. There is no consensus on the maximum number of shock waves [172]. Starting SWL on a lower energy setting with stepwise power (and SWL sequence) ramping can achieve vasoconstriction during treatment [168], which prevents renal injury [173-175]. Animal studies [176] and a prospective randomised study [177] have shown better SFRs (96% vs. 72%) using stepwise power ramping, but no difference has been found for fragmentation or evidence of complications after SWL, irrespective of whether ramping was used [178,179].
There are no conclusive data on the intervals required between repeated SWL sessions. However, clinical experience indicates that repeat sessions are feasible (within one day for ureteral stones) [180].
Improvement of acoustic coupling
Proper acoustic coupling between the cushion of the treatment head and the patient’s skin is important. Defects (air pockets) in the coupling gel deflect 99% of shock waves [181]. Ultrasound gel is probably the most widely-used agent available as a lithotripsy coupling agent [182].
Procedural control
Results of treatment are operator dependent, and experienced clinicians obtain better results. During the procedure, careful imaging control of localisation contributes to outcome quality [183].
Pain Control
Careful control of pain during treatment is necessary to limit pain-induced movements and excessive respiratory excursions [184-187].
Antibiotic prophylaxis
No standard antibiotic prophylaxis before SWL is recommended. However, prophylaxis is recommended in the case of internal stent placement ahead of anticipated treatments and in the presence of increased bacterial burden (e.g., indwelling catheter, nephrostomy tube, or infectious stones) [68,188,189].
Medical therapy after extracorporeal shock wave lithotripsy
Despite conflicting results, most RCTs and several MAs support MET after SWL for ureteral or renal stones as an adjunct to expedite expulsion and to increase SFRs. Medical expulsion therapy might also reduce analgesic requirements [190-199].
Post-treatment management
Mechanical percussion and diuretic therapy can significantly improve SFRs and accelerate stone passage after SWL [200-203].
Complications of extracorporeal shock wave lithotripsy
Compared to percutaneous nephrolithotomy (PNL) and ureteroscopy (URS), there are fewer overall complications with SWL [204,205] (Table 3.8). The relationship between SWL and hypertension or diabetes is unclear. Published data are contradictory; however, no evidence exists supporting the hypothesis that SWL may cause long-term adverse effects [206-212].
Table 3.8: Shock wave lithotripsy-related complications [213-227]
Complications | % | Reference | ||
Related to stone fragments | Steinstrasse | 4 – 7 | [225-227] | |
Regrowth of residual fragments | 21 – 59 | |||
Renal colic | 2 – 4 | [216] | ||
Infections | Bacteriuria in non-infection stones | 7.7 – 23 | ||
Sepsis | 1 – 2.7 | |||
Tissue effect | Renal | Haematoma, symptomatic | < 1 | [218] |
Haematoma, asymptomatic | 4 – 19 | [218] | ||
Cardiovascular | Dysrhythmia | 11 – 59 | ||
Morbid cardiac events | Case reports | |||
Gastrointestinal | Bowel perforation | Case reports | [220-222] | |
Liver, spleen haematoma | Case reports | |||
3.4.5.1. Summary of evidence and recommendations for SWL
Summary of evidence | LE |
Stepwise power ramping prevents renal injury. | 1b |
Clinical experience has shown that repeat sessions are feasible (within one day for ureteral stones). | 4 |
Optimal shock wave frequency is 1.0 to 1.5 Hz. | 1a |
Proper acoustic coupling between the cushion of the treatment head and the patient’s skin is important. | 2 |
Careful imaging control of localisation of stone contributes to outcome of treatment. | 2a |
Careful control of pain during treatment is necessary to limit pain-induced movements and excessive respiratory excursions. | 1a |
Antibiotic prophylaxis is recommended in the case of internal stent placement, infected stones, or bacteriuria. | 1a |
Recommendations | Strength rating |
Ensure correct use of the coupling agent because this is crucial for effective shock wave transportation. | Strong |
Maintain careful fluoroscopic and/or ultrasonographic monitoring during shock wave lithotripsy (SWL). | Strong |
Use proper analgesia because it improves treatment results by limiting pain-induced movements and excessive respiratory excursions. | Strong |
Prescribe antibiotics prior to SWL in the case of infected stones or bacteriuria. | Strong |
3.4.6. Ureteroscopy (retrograde and antegrade)
The current standard for rigid ureteroscopes is a tip diameter of < 8 French (F). Rigid URS can be used for the whole ureter [206]. However, technical improvements, as well as the availability of digital scopes, also favour the use of flexible ureteroscopes in the ureter [228].
Percutaneous antegrade removal of ureteral stones is a consideration in selected cases, i.e. large
(> 15 mm), impacted proximal ureteral calculi in a dilated renal collecting system [229-231], or when the ureter is not amenable to retrograde manipulation [231-235].
Ureteroscopy for renal stones (RIRS)
Technical improvements including endoscope miniaturisation, improved deflection mechanism, enhanced optical quality and tools, and introduction of disposables have led to an increased use of URS for both renal and ureteral stones. Major technological progress has been achieved for RIRS. A recent systematic review addressing renal stones > 2 cm showed a cumulative SFR of 91% with 1.45 procedures/patient; 4.5% of the complications were > Clavien 3 [228,236,237]. Digital scopes demonstrate shorter operation times due to the improvement in image quality [236].
Stones that cannot be extracted directly must be disintegrated. If it is difficult to access stones within the lower renal pole that need disintegration; it may help to displace them into a more accessible
calyx [238].
Best clinical practice in ureteroscopyAccess to the upper urinary tract
Most interventions are performed under general anaesthesia, although local or spinal anaesthesia is possible [239]. Intravenous sedation is suitable for female patients with distal ureteral stones [240]. Antegrade URS is an option for large, impacted, proximal ureteral calculi [229-231,241]. Reduction of flexible ureteroscope diameter may provide similar vision, deflection, and manoeuvrability to standard flexible ureteroscopes potentially with improved ureteric access [242]. Disposable ureteroscopes provides similar safety and clinical effectiveness to reusable scopes. Concerns regarding the cost effectiveness and environmental sustainability remain [243-245].
Safety aspects
Fluoroscopic equipment must be available in the operating room. The Panel recommend placement of a safety wire, even though some groups have demonstrated that URS can be performed without it [246-250]. Balloon and plastic dilators should be available, if necessary.
Prior rigid URS can be helpful for optical dilatation followed by flexible URS, if necessary. If ureteral access is not possible, insertion of a JJ stent followed by URS after seven to fourteen days offers an alternative [251]. Bilateral URS during the same session is feasible resulting in equivalent-to-lower SFRs, but slightly higher overall complication rates (mostly minor, Clavien 1 and 2) [252,253].
Difficult lower pole anatomy such as steep infundibulopelvic angle predisposes to failure during RIRS [254]. Prolonged operative times are linked to increased complication rates in ureteroscopy, and efforts must be made to keep it below 90 minutes [255].
Ureteral access sheaths
Hydrophilic-coated ureteral access sheaths, which are available in different calibres (inner diameter from 9 F upwards), can be inserted (via a guide wire) with the tip placed in the proximal ureter.
Ureteral access sheaths allow easy, multiple, access to the UUT and therefore significantly facilitate URS. The use of ureteral access sheaths improves vision by establishing a continuous outflow, decreases intrarenal pressure, and potentially reduces operating time [256,257].
The insertion of ureteral access sheaths may lead to ureteral damage, the risk is lowest in presented systems [258]. No data on long-term side effects are available [258,259]. Whilst larger cohort series showed no difference in SFRs and ureteral damage (stricture rates of about 1.8%), they did show lower post-operative infectious complications [260,261]. The use of ureteral access sheath is safe and can be useful for large and multiple renal stones or if long procedural time is expected [262].
Stone extraction
The aim of URS is complete stone removal. “Dust and go” strategies should be limited to the treatment of large (renal) stones [263]. Stones can be extracted by endoscopic forceps or baskets. Only baskets made of nitinol can be used for flexible URS [264].
Intracorporeal lithotripsy
The most effective lithotripsy system is the holmium: yttrium-aluminium-garnet (Ho:YAG) laser, which is currently the optimum standard for URS and flexible nephroscopy (Section 3.4.6), because it is effective in all stone types [265,266]. Compared to low-power lasers, high-power laser reduces procedural time although the reported difference in clinical outcomes were non-significant [267]. J Pneumatic and US systems can be used with high disintegration efficacy in rigid URS [268,269]. However, stone migration into the kidney is a common problem, which can be prevented by placement of special anti-migration tools proximal of the stone [270]. Medical expulsion therapy following Ho:YAG laser lithotripsy increases SFRs and reduces colic episodes [271]. Thulium fibre laser (TFL) for stone disease has a promising role, offers good clinical outcomes, which seem to be comparable to Ho:YAG laser (holmium) laser. More comparative clinical studies are however needed between these two modalities [272,273].
Stenting before and after URS
Routine stenting is not necessary before URS. Despite a complete lack of RCTs on this subject, a meta-analysis has been performed, demonstrating that pre-stenting may improve the stone free rate of ureteroscopic treatment of renal stones, but not of ureteral stones [274]. Although it may facilitate ureteroscopic management of stones and increase success in access sheath placement, intra-operative complications were not significantly different [274,275]. One should also take into account that pre-stenting also causes the patient to experience stent-related symptoms during the time the stent is indwelling, prior to a procedure.
Randomised prospective trials have found that routine stenting after uncomplicated URS (complete stone removal) is not necessary; stenting might be associated with higher post-operative morbidity and costs [276-279]. A ureteral catheter with a shorter indwelling time (one day) may also be used, with similar results [280].
Stents should be inserted in patients who are at increased risk of complications (e.g., ureteral trauma, residual fragments, bleeding, perforation, UTIs, or pregnancy), and in all doubtful cases, to avoid stressful emergencies. The ideal duration of stenting is not known. Most urologists favour one to two weeks after URS. Alpha-blockers reduce the morbidity of ureteral stents and increase tolerability [281,282].
Medical expulsive therapy before and after ureteroscopy
Medical expulsion therapy before URS might reduce the risk for intra-operative ureteral dilatation, protect against ureteral injury and increase stone free rates four weeks after URS [283]. Medical expulsion therapy following Ho:YAG laser lithotripsy accelerates the spontaneous passage of fragments and reduces episodes of colic [271].
Complications of ureteroscopy
The overall complication rate after URS is 9-25% [206,284,285]. Most complications are minor and do not require intervention. There is evidence suggesting a risk of post-operative urosepsis of up to 5% [286,287]. Ureteral avulsion and strictures are rare (< 1%). Previous perforations, pre-operative positive urine cultures and longer operation time are the most important risk factor for complications [255,288]. Infectious complications following URS can be minimised using prophylactic antibiotics, limiting stent dwell and procedural time, identification and treatment of UTI, and planning in patients with large stone burden and multiple comorbidities [289].
High intrarenal pressure (IRP) predisposes to URS complications, and measures should be used to reduce IRP. Currently there are no accurate ways to measure intra-operative IRP [290].
3.4.6.1. Summary of evidence and recommendations for retrograde URS, RIRS and antegrade ureteroscopy
Summary of evidence | LE |
In uncomplicated URS, a post-procedure stent need not be inserted. | 1a |
In URS, pre-stenting has been shown to improve outcomes only for renal stones. | 2a |
An α-blocker can reduce stent-related symptoms and colic episodes. | 1a |
The most effective lithotripsy system for flexible ureteroscopy is the Ho:YAG laser. | 2a |
Pneumatic and US systems can be used with high disintegration efficacy in rigid URS. | 2a |
Percutaneous antegrade removal of proximal ureter stones, or laparoscopic ureterolithotomy are feasible alternatives to retrograde ureteroscopy, in selected cases. | 1b |
Pre-treatment of patients undergoing URS with an α-blocker one week prior to the procedure reduces the need for active dilatation and increases the stone free rate. | 1a |
Recommendations | Strength rating |
Use holmium:yttrium-aluminium-garnet (Ho:YAG) laser lithotripsy for (flexible) ureteroscopy (URS). | Strong |
Perform stone extraction only under direct endoscopic visualisation of the stone. | Strong |
Do not insert a stent in uncomplicated cases. | Strong |
Offer medical expulsive therapy for patients suffering from stent-related symptoms and after Ho:YAG laser lithotripsy to facilitate the passage of fragments. | Strong |
Use percutaneous antegrade removal of ureteral stones as an alternative when shock wave lithotripsy (SWL) is not indicated or has failed, and when the upper urinary tract is not amenable to retrograde URS. | Strong |
Use flexible URS in cases where percutaneous nephrolithotomy or SWL are not an option (even for stones > 2 cm). However, in this case there is a higher risk that a follow-up procedure and placement of a ureteral stent may be needed. | Strong |
3.4.7. Percutaneous nephrolithotomy
Percutaneous nephrolithotomy remains the standard procedure for large renal calculi. Different rigid and flexible endoscopes are available, and the selection is mainly based on the surgeon’s own reference. Standard access tracts are 24-30 F. Smaller access sheaths, < 18 F, were initially introduced for paediatric use, but are now increasingly utilised in the adult population [291,292].
Contraindications
Patients receiving anti-coagulant therapy must be monitored carefully pre- and post-operatively. Anti-coagulant therapy must be discontinued before PNL [293].
Other important contraindications include:
- untreated UTI;
- tumour in the presumptive access tract area;
- potential malignant kidney tumour;
- pregnancy (Section 3.4.14.1).
Best clinical practiceIntracorporeal lithotripsy
Several methods for intracorporeal lithotripsy during PNL are available. Ultrasonic and pneumatic systems are most commonly used for rigid nephroscopy, whilst laser is increasingly used for miniaturised instruments [294]. Flexible endoscopes also require laser lithotripsy to maintain tip deflection, with the Ho:YAG laser having become the standard.
Pre-operative imaging
Pre-procedural imaging evaluations are summarised in Section 3.3.1. In particular, US or CT of the kidney and the surrounding structures can provide information regarding interposed organs within the planned percutaneous path (e.g., spleen, liver, large bowel, pleura, and lung).
Positioning of the patient
Both prone and supine positions are equally safe, although the supine position confers some advantages, it depends on appropriate equipment being available to position the patient correctly, for example, X-ray devices and an operating table. A meta-analysis including 12 studies and a total of 1,290 patients treated, showed a similar SFR but a lower operative time for supine PNL [295]. Prone position offers more options for puncture and is therefore preferred for upper pole or multiple accesses [296,297]. On the other hand, supine position allows simultaneous retrograde access to the collecting system, using flexible ureteroscope [298]. The combination of PNL and RIRS may be a good alternative for the treatment of complex renal stones compared to standard PNL; however, the existing evidence is of low quality [295].
Puncture
Although fluoroscopy is the most common intra-operative imaging method, the (additional) use of US reduces radiation exposure [299-301]. Pre-operative CT or intra-operative US allows identification of the tissue between the skin and kidney and lowers the incidence of visceral injury. The calyceal puncture may be done under direct visualisation using simultaneous flexible URS [300,302,303].
Dilatation
Dilatation of the percutaneous access tract can be achieved using a metallic telescope, single (one-shot or serial) dilators, or a balloon dilatator. During PNL, safety and effectiveness are similar for different tract dilatation methods [304]. Although there are papers demonstrating that single step dilation is equally effective as other methods and that US only can be used for the dilatation, the difference in outcomes is most likely related to surgeon experience rather than to the technology used [304,305]. A meta-analysis on the most commonly used tract dilation methods suggested that one-step dilation would allow for a shorter operative time and reduced complication rate, including haemoglobin loss and transfusion rate [306].
Choice of instruments
Several meta-analyses on mPNL (12-22 F) vs. standard PNL (> 22 F) have identified that both techniques allow for a similar SFR. Patients treated with mPNL had reduced blood loss and transfusion rates, as well as shorter hospital stays, without a significant difference in overall complication rates [292,307-309]. However, it is important to note that the level of evidence was downgraded due to heterogeneity of data related to tract sizes used and types of stones treated. There is some evidence for using suction during PNL to reduce IRP and increase SFR [310].
Nephrostomy and stents
The decision on whether, or not, to place a nephrostomy tube at the conclusion of the PNL procedure depends on several factors, including:
- presence of residual stones;
- likelihood of a second-look procedure;
- significant intra-operative blood loss;
- urine extravasation;
- ureteral obstruction;
- potential persistent bacteriuria due to infected stones;
- solitary kidney;
- bleeding diathesis;
- planned percutaneous chemolitholysis.
Small-bore nephrostomies seem to have advantages in terms of post-operative pain [292,311,312]. Tubeless PNL is performed without a nephrostomy tube and is associated with reduced post-operative pain and hospital stay [313]. When neither a nephrostomy tube nor a ureteral stent is introduced, the procedure is known as totally tubeless PNL [314]. In uncomplicated cases, the latter procedure results in a shorter hospital stay, with no disadvantages reported [315].
Complications of percutaneous nephrolithotomy
A systematic review of almost 12,000 patients shows the incidence of complications associated with PNL; fever 10.8%, transfusion 7%, thoracic complication 1.5%, sepsis 0.5%, organ injury 0.4%, embolisation 0.4%, urinoma 0.2%, and death 0.05% [316].
Peri-operative fever can occur, even with a sterile pre-operative urinary culture and peri-operative antibiotic prophylaxis, because the renal stones themselves may be a source of infection. The evidence demonstrates that a stone culture or urine culture taken directly from the renal pelvis is more predictive of post-operative systemic inflammatory response syndrome (SIRS) or sepsis. Whenever possible a urine culture from the renal pelvis and/or stone culture should be taken at time of percutaneous cystolithotripsy [317].
Intra-operative renal stone or renal pelvic urine culture may be more indicative of the causative organism for sepsis; therefore, helping to select the most suitable post-operative antibiotics [317-319]. Intra-operative irrigation pressure < 30 mmHg and unobstructed post-operative urinary drainage may be important factors in preventing post-operative sepsis [320]. Bleeding after PNL may be treated by briefly clamping the nephrostomy tube. Super-selective embolic occlusion of the arterial branch may become necessary in the case of severe bleeding. The use of tranexamic acid seems to reduce bleeding complications and transfusion rate of PNL; however, more evidence is needed before it can be introduced in routine clinical practice [321,322].
To reduce post-operative pain after PNL, a peripheral nerve block can be performed at the intercostal nerve, paravertebral region, erector spinae or quadratus lumborum. Such a block may significantly reduce the need for post-operative opioid analgesics [323].
High IRP predisposes to PNL complications, and measures should be taken to reduce IRP. Currently there are no accurate ways to measure IRP [290].
3.4.7.1. Summary of evidence and recommendations for endourology techniques for renal stone removal
Summary of evidence | LE |
Imaging of the kidney with US or CT can provide information regarding inter-positioned organs within the planned percutaneous path (e.g., spleen, liver, large bowel, pleura, and lung). | 1a |
Both prone and supine positions are equally safe with equivalent SFR. | 1a |
Percutaneous nephrolithotomy performed with small instruments tends to be associated with significantly lower blood loss, but the duration of procedure tended to be significantly longer. There are no significant differences in SFR or any other complications. | 1a |
In uncomplicated cases, a totally tubeless PNL results in a shorter hospital stay, with no increase in complication rate. | 1a |
Peri-operative use of tranexamic acid may reduce bleeding complications and transfusion rates. | 1a |
Urine culture taken directly from the renal pelvis or a stone culture are more predictive of post-PNL sepsis than a pre-operative midstream urine culture. | 1a |
Recommendations | Strength rating |
Perform pre-procedural imaging, including contrast medium where possible or retrograde study when starting the procedure, to assess stone comprehensiveness and anatomy of the collecting system to ensure safe access to the renal stone. | Strong |
Perform a tubeless (without nephrostomy tube) or totally tubeless (without nephrostomy tube and ureteral stent) percutaneous nephrolithotomy (PNL) procedure, in uncomplicated cases. | Strong |
Take a stone culture or urine culture directly from the renal pelvis at time of PNL, if possible. | Strong |
3.4.8. General recommendations and precautions for stone removal
3.4.8.1. Antibiotic therapy
Urinary tract infections should always be treated if stone removal is planned. In patients with clinically significant infection and obstruction, drainage should be performed for several days before starting stone removal. A urine culture or urinary microscopy should be performed before treatment [324].
Peri-operative antibiotic prophylaxis
For prevention of infection following URS and percutaneous stone removal, no clear-cut evidence exists [289,325]. In a review of a large database of patients undergoing PNL, it was found that in patients with negative baseline urine culture, antibiotic prophylaxis significantly reduced the rate of post-operative fever and other complications [326]. Single dose administration prior to ureteroscopy was found to be sufficient [327]. Based on a meta-analysis by Yu et al., an extended course of pre-operative prophylactic antibiotics prior to PNL compared to single dose before anaesthesia significantly reduced post-operative sepsis and fever [318]. In an RCT including only moderate to high-risk of infection patients (patients with pre-operative stents/nephrostomy or positive urine culture), a seven-day course of pre-operative antibiotics reduced the risk of post-PNL sepsis threefold in comparison to a two-day course. In studies that did not specify the risk of the patient population, a single dose of antibiotic prophylaxis administered at induction was equivalent to an extended pre-operative course [328]. In contrast to this, a prolonged course of post-operative antibiotics was not superior to a single dose pre-operatively [318,329].
As national and regional antibiotic resistance patterns can differ significantly, the choice of antibiotic prophylaxis should be tailored to institutional or regional antimicrobial susceptibility [330].
Recommendations | Strength rating |
Obtain a urine culture or perform urinary microscopy before any treatment is planned. | Strong |
Exclude or treat urinary tract infections prior to stone removal. | Strong |
Offer peri-operative antibiotic prophylaxis to all patients undergoing endourological treatment. | Strong |
3.4.8.2. Antithrombotic therapy and stone treatment
Patients with a bleeding disorder, or receiving antithrombotic therapy, should be referred to an internist for appropriate therapeutic measures before deciding on stone management [331-335]. In patients with an uncorrected bleeding disorder, the following are at elevated risk of haemorrhage or perinephric haematoma (PNH) (high-risk procedures):
- SWL (hazard ratio of PNH up to 4.2 during anti-coagulant/anti-platelet medication [336-338]);
- PNL;
- percutaneous nephrostomy;
- laparoscopic surgery;
- open surgery [331].
Shock wave lithotripsy is feasible and safe after correction of the underlying coagulopathy [339-343]. In the case of an uncorrected bleeding disorder or continued antithrombotic therapy, URS, in contrast to SWL and PNL, might offer an alternative approach since it is associated with less morbidity [344-346]. Despite appropriate cessation of anti-platelet agents, following standardised protocols, prolonged haematuria in tube drainage after PNL has been reported [347]. Only data on flexible URS are available which support the superiority of URS in the treatment of proximal ureteral stones [348,349]. Although URS is safe in patients with bleeding disorders or anticoagulation, an individualised patient-approach is necessary [346].
Table 3.9: Risk stratification for bleeding [333-335, 350]
Low-risk bleeding procedures | Cystoscopy Flexible cystoscopy Ureteral catheterisation Extraction of ureteral stent Ureteroscopy |
High-risk bleeding procedures | Shock wave lithotripsy Percutaneous nephrostomy Percutaneous nephrolithotomy |
Table 3.10: Suggested strategy for antithrombotic therapy in stone removal [333-335]
(In collaboration with a cardiologist/internist weigh the risks and benefits of discontinuation of therapy, vs. delaying elective surgical procedures).
Medication/Agent | Bleeding risk of planned procedure | Risk of thromboembolism | ||
Low risk | Intermediate risk | High risk | ||
Warfarin Dabigatran Rivaroxaban Apixaban | Low-risk procedure | May be continued | Bridging therapy | Bridging therapy |
High-risk procedure | May be temporarily discontinued at appropriate interval. Bridging therapy is strongly recommended. | Bridging therapy | Bridging therapy | |
Aspirin | Low-risk procedure | Continue | Continue | Elective surgery: postpone. Non-deferrable surgery: continue. |
High-risk procedure | Discontinue | Elective surgery: postpone. Non-deferrable surgery: continue, if it is possible. | Elective surgery: postpone. Non-deferrable surgery: continue. | |
Thienopyridine agents (P2Y12 receptor inhibitors) | Low-risk procedure | Discontinue five days before intervention. Resume within 24-72 hours with a loading dose. | Continue | Elective surgery: postpone. Non-deferrable surgery: continue. |
High-risk procedure | Discontinue five days before intervention and resume within 24-72 hours with a loading dose. | Elective surgery: postpone. Non-deferrable surgery: discontinue five days before procedure and resume within 24-72 hours with a loading dose. Bridging therapy -glycoprotein IIb/IIIa inhibitors if aspirin is discontinued. | Elective surgery: postpone. Non-deferrable surgery: discontinue five days before procedure and resume within 24-72 hours, with a loading dose. Bridging therapy -glycoprotein IIb/IIIa inhibitors. | |
3.4.8.2.1. Summary of evidence and recommendations for antithrombotic therapy and stone treatment
Summary of evidence | LE |
Active surveillance is indicated in patients at high risk for thrombotic complications in the presence of an asymptomatic calyceal stone. | 4 |
The temporary discontinuation, or bridging of antithrombotic therapy in high-risk patients, should be discussed with the internist. | 3 |
Retrograde (flexible) URS stone removal is associated with less morbidity in patients when antithrombotic therapy cannot be discontinued. | 2a |
Recommendations | Strength rating |
Offer active surveillance to patients at high risk of thrombotic complications in the presence of an asymptomatic calyceal stone. | Weak |
Decide on temporary discontinuation, or bridging of antithrombotic therapy in high-risk patients, in consultation with the internist. | Strong |
Retrograde (flexible) ureteroscopy is the preferred intervention if stone removal is essential and antithrombotic therapy cannot be discontinued since it is associated with less morbidity. | Strong |
3.4.8.3. Obesity
A high BMI can pose a higher anaesthetic risk and a lower success rate after SWL and PNL and may influence the choice of treatment [351].
3.4.8.4. Stone composition
Stones composed of brushite, calcium oxalate monohydrate, or cystine are particularly hard, as well as homogeneous stones with a high density on NCCT [46,352]. Percutaneous nephrolithotomy or RIRS and URS are alternatives for removal of large SWL-resistant stones.
Recommendations | Strength rating |
Consider the stone composition before deciding on the method of removal, based on patient history, former stone analysis of the patient or Hounsfield unit on unenhanced computed tomography. | Strong |
Attempt to dissolve radiolucent stones. | Strong |
3.4.8.5. Contraindications of procedures
Contraindications of extracorporeal SWL
There are several contraindications to the use of extracorporeal SWL, including:
- pregnancy, due to the potential effects on the foetus [353];
- bleeding disorders, which should be compensated for at least 24 hours before and 48 hours after treatment [354];
- uncontrolled UTIs;
- severe skeletal malformations and severe obesity, which prevent targeting of the stone;
- arterial aneurysm in the vicinity of the stone [355];
- anatomical obstruction distal to the stone.
Contraindications of URS
Apart from general problems, for example with general anaesthesia or untreated UTIs, URS can be performed in all patients without any specific contraindications.
Contraindications of PNL
Patients receiving anti-coagulant therapy must be monitored carefully pre- and post-operatively. Anti-coagulant therapy must be discontinued before PNL [346]. Other important contraindications include:
- untreated UTI;
- tumour in the presumptive access tract area;
- potential malignant kidney tumour;
- pregnancy (Section 3.4.14.1).
General contraindication for endourological procedures
Endourological interventions do not adversely affect renal function although care must be taken in those with poor pre-operative renal function, diabetes and hypertension [356]. However, a meta-analysis, based on low- quality evidence, suggests that patients with impaired renal function and stone disease, may in fact benefit from the procedure to preserve or increase their renal function [357].
3.4.9. Specific stone management of ureteral stones
3.4.9.1. Conservative treatment/observation
There are only limited data regarding spontaneous stone passage according to stone size [358]. It is estimated that 95% of stones up to 4 mm pass within 40 days [206].
Based on an analysis of available evidence, an exact cut-off size for stones that are likely to pass spontaneously cannot be provided [206].
Spontaneous stone passage was reported for 49% of upper ureteral stones, 58% of mid ureteral stones and 68% of distal ureteral stones. Considering stone size almost 75% of stones < 5 mm and 62% of stones > 5 mm passed spontaneously, with an average time to stone expulsion about 17 days (range 6-29 days) [359]. The Panel is aware of the fact that spontaneous stone expulsion decreases with increasing stone size and that there are differences between individual patients.
According to a number of RCT based meta-analysis sexual intercourse has been reported to be beneficial in facilitating stone expulsion in men with distal ureteral stones and be comparable to MET [360-362].
3.4.9.2. Pharmacological treatment, medical expulsive therapy
Medical expulsive therapy should only be used in informed patients if active stone removal is not indicated. Treatment should be discontinued if complications develop (infection, refractory pain, deterioration of renal function). In case of known uric acid stones in the distal ureter, a combination of alkalinisation with tamsulosin can increase the frequency of spontaneous passage. For details see Sections 3.4.3 and 3.4.4.
3.4.9.3.Indications for active removal of ureteral stones
Indications for active removal of ureteral stones are [206,358,363]:
- stones with a low likelihood of spontaneous passage;
- persistent pain despite adequate analgesic medication;
- persistent obstruction;
- renal insufficiency (renal failure, bilateral obstruction, or single kidney).
3.4.9.4. Selection of procedure for active removal of ureteral stones
Overall, SFRs after URS or SWL for ureteral stones are comparable. However, larger stones achieve earlier stone-free status with URS.
A large multi-center non-inferiority trial compared URS to ESWL for ureteral stones. When excluding patients that had spontaneously passed their stone prior to treatment, ESWL could not be considered non-inferior to URS with only 12% of patients needing further intervention after URS in comparison to 26% in the SWL arm [364]. In the current endourological era, the complication rate and morbidity of URS has been significantly reduced [365]. It has been demonstrated that URS is a safe option in obese patients (BMI > 30 kg/m2) with comparable SFRs
and complication rates. However, in morbidly obese patients (BMI > 35 kg/m2) the overall complication rates double [366].
The Panel performed a systematic review to assess the benefits and harms of URS compared to SWL [367]. Compared with SWL, URS was associated with a significantly greater SFR of up to four weeks, but the difference was not significant at three months in the included studies. Ureteroscopy was associated with fewer retreatments and need for secondary procedures, but with a higher need for adjunctive procedures, greater complication rates and longer hospital stay. Counterbalancing for URS’s higher SFRs, SWL is associated with lower morbidity. Success rates and complications of URS are not impacted by previous unsuccessful SWL [368]. Clavien-Dindo grade complications were, if reported, less frequent in patients treated with SWL [369].
Bleeding disorder
Ureteroscopy can be performed in patients with bleeding disorders, with a moderate increase in complications (see also Section 3.4.8.2) [346].
3.4.9.4.1. Summary of evidence and recommendations for selection of procedure for active removal of ureteral stones
Summary of evidence | LE |
Observation is feasible in informed patients who develop no complications (infection, refractory pain, deterioration of renal function). | 1a |
Medical expulsive therapy seems to be efficacious for treating patients with ureteral stones who are amenable to conservative management. The greatest benefit might be among those with > 5 mm (distal) stones. | 1a |
Compared with SWL, URS was associated with significantly greater SFRs up to four weeks, but the difference was not significant at three months in the included studies. | 1a |
Ureteroscopy was associated with fewer retreatments and need for secondary procedures, but with a higher need for adjunctive procedures, greater complication rates and longer hospital stay. | 1a |
In the case of severe obesity, URS is a more promising therapeutic option than SWL. | 2b |
Recommendations | Strength rating |
If active removal is not indicated (Section 3.4.9.3) in patients with newly diagnosed small* ureteral stones, observe patient initially with periodic evaluation. | Strong |
Offer α-blockers as medical expulsive therapy as one of the treatment options for (distal) ureteral stones > 5 mm. | Strong |
Inform patients that ureteroscopy (URS) has a better chance of achieving stone-free status with a single procedure. | Strong |
Inform patients that URS has higher complication rates when compared to shock wave lithotripsy. | Strong |
Use URS as first-line therapy for ureteral (and renal) stones in cases of severe obesity. | Strong |
*See stratification data [206].
Figure 3.1: Treatment algorithm for ureteral stones (if active stone removal is indicated)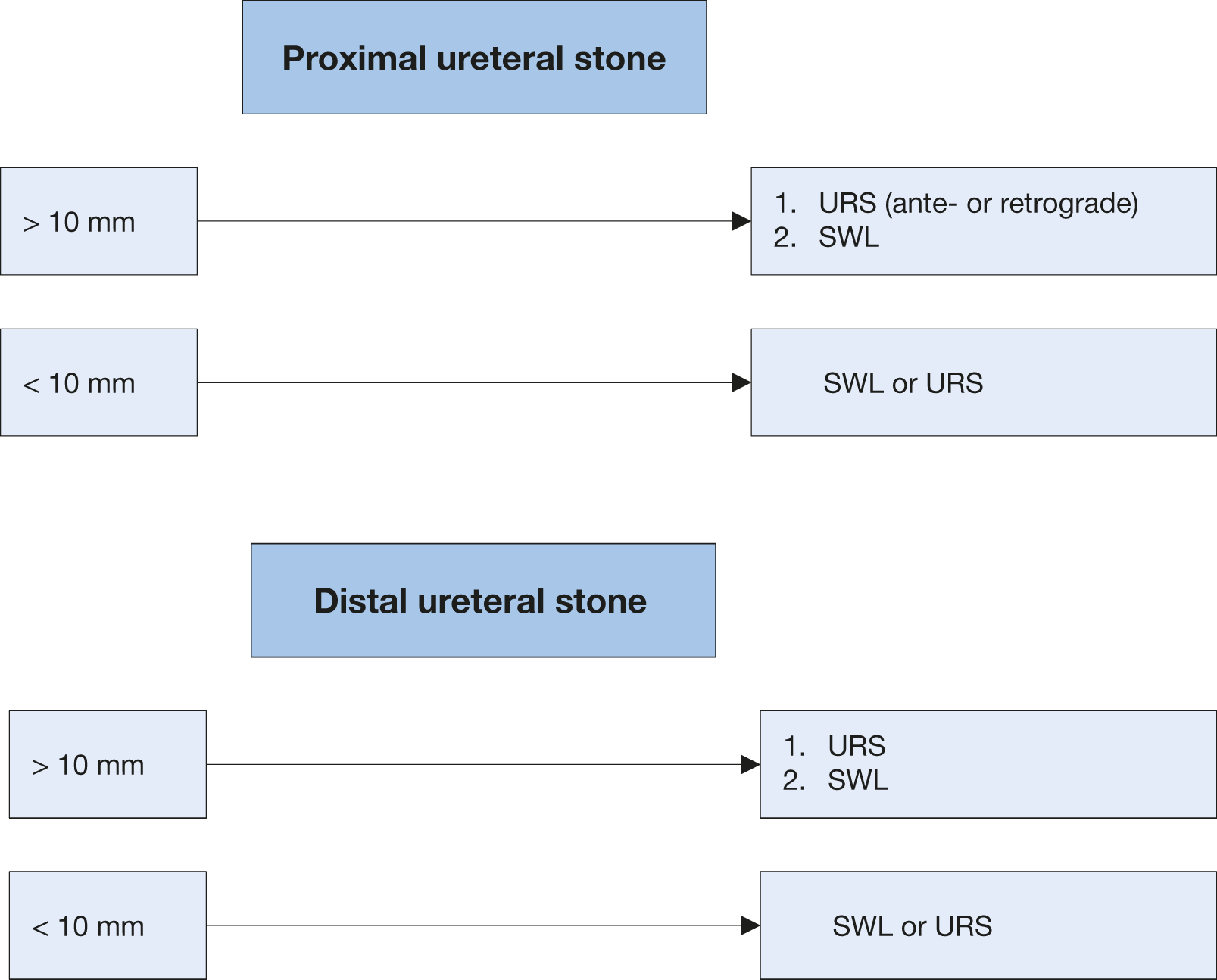 SWL = shock wave lithotripsy; URS = Ureteroscopy.
SWL = shock wave lithotripsy; URS = Ureteroscopy.
3.4.10. Specific stone management of renal stones
The natural history of small, non-obstructing asymptomatic calculi is not well defined, and the risk of
progression is unclear. There is still no consensus on the follow-up duration, timing, and type of intervention. Treatment options are chemolysis or active stone removal.
3.4.10.1. Conservative treatment (observation)
Observation of renal stones, especially in calyces, depends on their natural history (Section 3.4.10.3). The recommendations provided are not supported by high-level literature [370]. There is a prospective trial supporting annual observation for asymptomatic inferior calyceal stones, < 10 mm. In case stone growth is detected, the follow-up interval should be lowered. Intervention is advised for growing stones > 5 mm [371]. In a systematic review of patients with asymptomatic renal stones on active surveillance spontaneous stone passage rates varied from 3-29%, symptom development from 7-77%, stone growth from 5-66%, surgical intervention from 7-26% [370], respective risk of symptomatic episodes ranged from 0-59.4% [372].
3.4.10.2. Pharmacological treatment of renal stones
Dissolution of stones through pharmacological treatment is an option for uric acid stones only, but information on the composition of the stone will need to guide the type of treatment selected. See sections 3.4.4. and 3.4.8.4.
3.4.10.3. Indications for active stone removal of renal stones
Indications for the removal of renal stones, include:
- stone growth;
- stones in high-risk patients for stone formation;
- obstruction caused by stones;
- infection;
- symptomatic stones (e.g., pain or haematuria) [373];
- stones > 15 mm;
- stones < 15 mm if observation is not the option of choice;
- patient preference;
- comorbidity;
- social situation of the patient (e.g., profession or travelling);
- choice of treatment.
The risk of a symptomatic episode or need for intervention in patients with asymptomatic renal stones seems to be ~10-25% per year, with a cumulative five-year event probability of 48.5% [371,372,374,375]. A prospective RCT with more than two years clinical follow-up reported no significant difference between SWL and observation when comparing asymptomatic calyceal stones < 15 mm in terms of SFR, symptoms, requirement for additional treatment, quality of life (QoL), renal function, or hospital admission [376]. Although some have recommended prophylaxis for these stones to prevent renal colic, haematuria, infection, or stone growth, conflicting data have been reported [375,377,378]. In a follow-up period of almost five years after SWL, two series have demonstrated that up to 25% of patients with small residual fragments needed treatment [215,379]. Although the question of whether calyceal stones should be treated is still unanswered, stone growth, de novo obstruction, associated infection, and acute and/or chronic pain are indications for treatment [373,380,381]. There is some evidence that external physical vibration lithecbole (EPVL) after SWL and RIRS results in higher SFRs [203].
3.4.10.4. Selection of procedure for active removal of renal stones
For general recommendations and precautions see Section 3.4.8.
3.4.10.4.1. Stones in renal pelvis or upper/middle calyces
Shock wave lithotripsy, PNL and RIRS are available treatment modalities for renal calculi. While PNL efficacy is hardly affected by stone size, the SFRs after SWL or URS are inversely proportional to stone size [364,382-388]. Although multiple treatments or sessions may be needed SWL achieves good SFRs for stones up to 20 mm, except for those at the lower pole [384,389,390]. Endourology is considered an alternative because of the reduced need for repeated procedures and consequently a shorter time until stone-free status is achieved. For stones > 10 mm, mini-PNL (mPNL) achieves a higher SFR than RIRS or ESWL, but carries a higher risk of bleeding and is associated with a longer hospital stay; however, there is a high degree of heterogeneity among the included studies [386,388]. Stones > 20 mm should be treated primarily by PNL, because SWL often requires multiple treatments, and is associated with an increased risk of ureteral obstruction (colic or steinstrasse) with a need for adjunctive procedures (Figure 3.2) [204]. Retrograde renal surgery cannot be recommended as first-line treatment for stones > 20 mm in uncomplicated cases as SFRs decrease, and staged procedures will be required [391-393]. However, it may be a first-line option in patients where PNL is not an option or contraindicated or in selected patients [394]. The combination of PNL and RIRS may be a good alternative for the treatment of complex renal stones compared to standard PNL; however, the level of the existing evidence is low [295].
3.4.10.4.2. Stones in the lower renal pole
The stone clearance rate after SWL seems to be lower for stones in the inferior calyx than for other intra-renal locations. Although the disintegration efficacy of SWL is not limited compared to other locations, the fragments often remain in the calyx and cause recurrent stone formation. The reported SFR of SWL for lower pole calculi is 25-95%. The preferential use of endoscopic procedures is supported by some current reports, even for stones < 1 cm [204,382,383,385,389,393,395-407].
The following can impair successful stone treatment by SWL [397,408-413]:
- steep infundibular-pelvic angle;
- long calyx;
- long skin-to-stone distance;
- narrow infundibulum;
- shock wave-resistant stones (calcium oxalate monohydrate, brushite, or cystine).
Further anatomical parameters cannot yet be established. Supportive measures such as inversion, vibration or hydration may facilitate stone clearance (See 3.4.5 ESWL) [201,203,414]. If there are negative predictors for SWL, PNL and RIRS might be reasonable alternatives, even for smaller calculi [395]. Retrograde renal surgery seems to have comparable efficacy to SWL [204,383,389,415]. Recent clinical experience has suggested a higher SFR of RIRS compared to SWL, but at the expense of greater invasiveness. Depending on operator skills, stones up to 3 cm can be treated by RIRS [237,416-418]. However, staged procedures are frequently required. Although mPNL has the highest success rate for the treatment of lower pole stones up to 2 cm, it comes at the expense of a higher complication rate and longer hospital stay [388].
In complex stone cases, open or laparoscopic approaches are possible alternatives although they are infrequently used.
3.4.10.5. Summary of evidence and recommendations for the management of renal stones
Summary of evidence | LE |
It is still debatable whether renal stones should be treated, or whether annual follow-up is sufficient for asymptomatic calyceal stones that have remained stable for six months. | 4 |
Although the question of whether asymptomatic calyceal stones should be treated is still unanswered, stone growth, de novo obstruction, associated infection, and acute and/or chronic pain are indications for treatment. | 3 |
Percutaneous nephrolithotomy is indicated in renal stones > 2 cm as primary option. | 1a |
Recommendations | Strength rating |
Follow-up periodically in cases where renal stones are not treated (initially after six months then yearly evaluating symptoms and stone status either by ultrasound or kidney-ureter bladder radiography. Use computed tomography (CT) when intervention is required. | Strong |
Offer active treatment for renal stones in case of stone growth, de novo obstruction, associated infection, and acute and/or chronic pain. | Weak |
Evaluate stone composition before deciding on the method of removal, based on patient history, former stone analysis of the patient or Hounsfield unit (HU) on unenhanced CT. Stones with density > 1,000 HU (and with high homogeneity) on non-contrast-enhanced CT are less likely to be disintegrated by shock wave lithotripsy. | Strong |
Perform percutaneous nephrolithotomy (PNL) as first-line treatment of larger stones > 2 cm. | Strong |
Treat larger stones (> 2 cm) with flexible ureteroscopy or shock wave lithotripsy (SWL), in cases where PNL is not an option. However, in such instances there is a higher risk that a follow-up procedure and placement of a ureteral stent may be needed. | Strong |
Perform PNL or retrograde intrarenal surgery for the lower pole, even for stones > 1 cm, as the efficacy of SWL is limited (depending on favourable and unfavourable factors for SWL). | Strong |
Figure 3.2: Treatment algorithm for renal stones (if/when active treatment is indicated)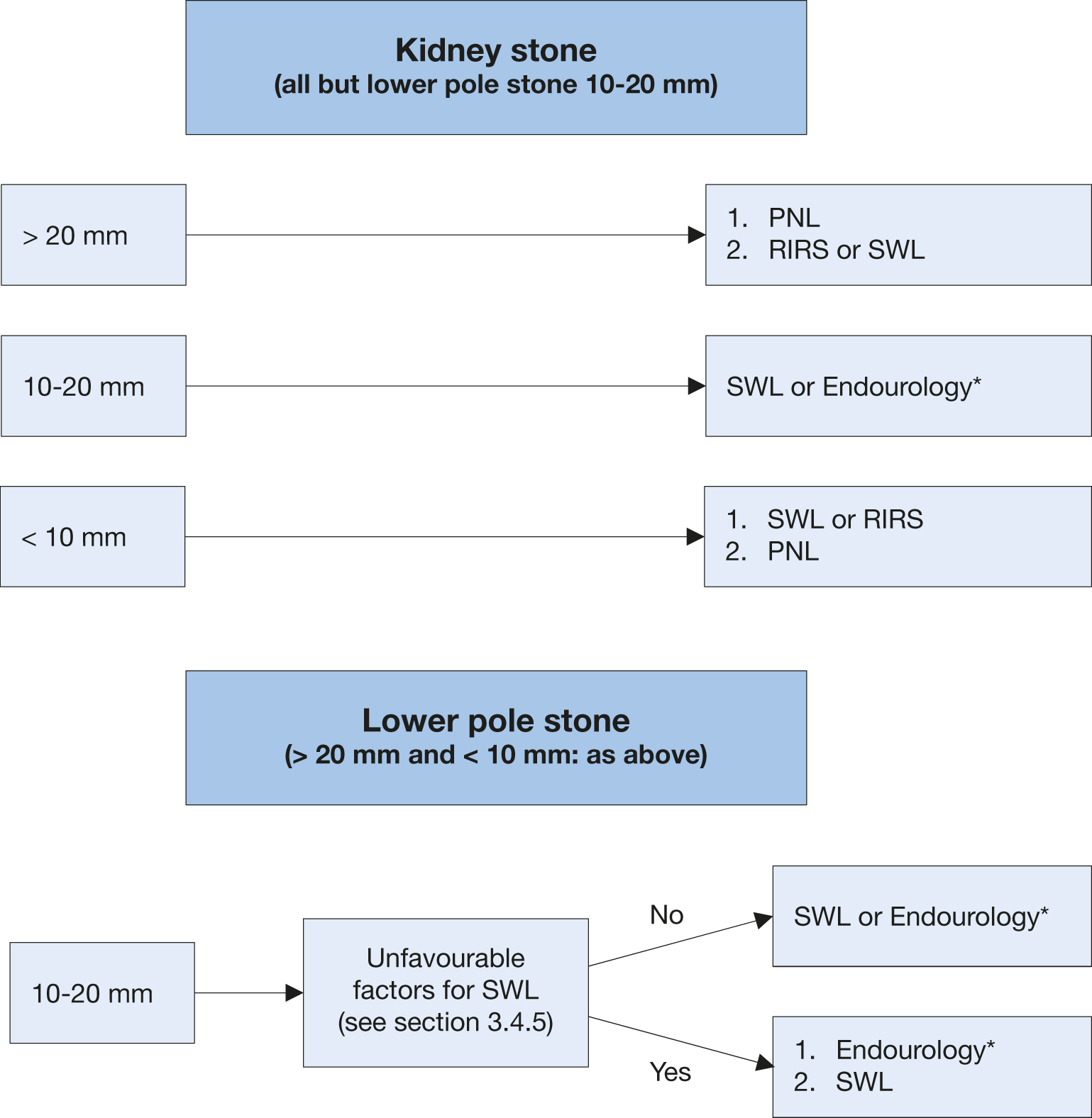 *The term ‘Endourology’ encompasses all PNL and URS interventions.
*The term ‘Endourology’ encompasses all PNL and URS interventions.
PNL = percutaneous nephrolithotomy; RIRS = retrograde intrarenal surgery; SWL = shock wave lithotripsy; URS = ureteroscopy.
3.4.11. Laparoscopy and open surgery
Advances in SWL and endourological surgery (URS and PNL) have significantly decreased the indications for open or laparoscopic stone surgery [419-424]. There is a consensus that most complex stones, including partial and complete staghorn stones, should be approached primarily with PNL. Additionally, a combined approach with PNL and RIRS may also be an appropriate alternative. However, if percutaneous approaches are not likely to be successful, or if multiple endourological approaches have been performed unsuccessfully; open or laparoscopic surgery may be a valid treatment option [425-431].
Few studies have reported laparoscopic stone removal. These procedures are usually reserved for special cases. When expertise is available, laparoscopic ureterolithotomy can be performed for large proximal ureteral stones as an alternative to URS or SWL [432,433]. These more invasive procedures have yielded high SFRs and lower auxiliary procedure rates [230,241,434]. A recent systematic review showed no difference in the post-operative phase for stented or unstented laparoscopic ureterolithotomy [434].
Laparoscopic pyelolithotomy could be offered for solitary stones > 2cm located in renal pelvis as an alternative to PNL [435]. In addition, in selected cases with an extrarenal and dilated pelvis, retroperitoneal laparoscopic pyelolithotomy (RLP) can be considered as an alternative management of staghorn calculi [436].
A few studies with limited numbers of patients have reported using robotic surgery in the treatment of urinary stones [437]. Open surgery should be considered as the last treatment option, after all other possibilities have been explored.
Studies on laparoscopy should be interpreted with caution due to their poor design and low quality of evidence.
3.4.11.1. Recommendation for laparoscopy and open surgery
Recommendation | Strength rating |
Offer laparoscopic or open surgical stone removal in rare cases in which shock wave lithotripsy, retrograde or antegrade ureteroscopy and percutaneous nephrolithotomy fail, or are unlikely to be successful. | Strong |
3.4.12. Steinstrasse
Steinstrasse is an accumulation of stone fragments or stone gravel in the ureter and may interfere with the passage of urine [438]. Steinstrasse occurs in 4-7% cases of SWL [225], and the major factor in the development of steinstrasse formation is stone size [439].
A major problem of steinstrasse is ureteral obstruction, which may be silent in up to 23% of cases. A MA including eight RCTs (n = 876) suggested a benefit of stenting before SWL in terms of steinstrasse formation, but did not result in a benefit on SFRs or less auxiliary treatments [154]. When steinstrasse is asymptomatic, conservative treatment is an initial option. Medical expulsion therapy increases stone expulsion and reduces the need for endoscopic intervention [440,441]. Ureteroscopy and SWL are effective in treatment of steinstrasse [227,442]. In the event of UTI or fever, the urinary system should be decompressed, preferably by percutaneous nephrostomy [125,129].
3.4.12.1. Summary of evidence and recommendations for steinstrasse
Summary of evidence | LE |
Medical expulsion therapy increases the stone expulsion rate of steinstrasse. | 1b |
Ureteroscopy is effective for the treatment of steinstrasse. | 3 |
Only low-level evidence is available, supporting SWL or URS for the treatment of steinstrasse. | 4 |
Recommendations | Strength rating |
Treat steinstrasse associated with urinary tract infection (UTI)/fever preferably with percutaneous nephrostomy. | Weak |
Treat steinstrasse when large stone fragments are present with shock wave lithotripsy or ureteroscopy (in absence of signs of UTI). | Weak |
3.4.13. Management of patients with residual stones
Following initial treatment with SWL, URS or PNL, residual fragments may remain and require additional intervention [372,379,443-445]. Most of the studies indicate that initial imaging is performed on the first day or the first week after treatment. However, false positive results from dust or residual fragments, that will pass spontaneously without causing any stone-related event, might lead to over-treatment. Therefore, imaging at four weeks seems most appropriate [446-448]. Compared to US, KUB and IVU, NCCT scan has a higher sensitivity to detect small residual fragments after definitive treatment of ureteral or kidney stones [449,450]. However, more than half of the patients with a residual fragment on NCCT images may not experience a stone-related event [451].
It is clear that NCCT has the highest sensitivity to detect residual fragments; however, this must be balanced against the increased detection of clinically insignificant fragments and the exposure to ionising radiation when compared with KUB and US. In the absence of high-level supporting evidence, the timing of follow-up imaging studies and need for secondary intervention is left to the discretion of the treating physician. Recurrence risk in patients with residual fragments after treatment of infection stones is higher than for other stones [452]. For all stone compositions, 21-59% of patients with residual stones required treatment within five years. Fragments > 5 mm are more likely than smaller ones to require intervention [215,372,445,453,454]. There is evidence that fragments > 2 mm are more likely to grow, although this is not associated with increased re-intervention rates at one year follow up [443].
3.4.13.1. Summary of evidence and recommendation for management of patients with residual stones
Summary of evidence | LE |
To detect residual fragments after SWL, URS or PNL, deferred imaging is more appropriate than immediate imaging post intervention. | 3 |
Recommendation | Strength rating |
Perform imaging after shock wave lithotripsy, ureteroscopy or percutaneous antegrade ureteroscopy to determine presence of residual fragments. | Strong |
3.4.14. Management of specific patient groups
3.4.14.1. Management of urinary stones and related problems during pregnancy
Clinical management of a pregnant urolithiasis patient is complex and demands close collaboration between patient, radiologist, obstetrician, and urologist [70]. For diagnostic imaging see Section 3.3.1. Patients with urolithiasis may be at increased risk of developing adverse maternal or neonatal outcomes [455].
If spontaneous passage does not occur, or if complications develop (e.g., intractable symptoms, severe hydronephrosis, spontaneous renal fornix rupture [456] or induction of premature labour), placement of a ureteral stent or a percutaneous nephrostomy tube is necessary as it is more effective than conservative treatment for symptom relief [127,457,458].
Unfortunately, these temporising therapies are often associated with poor tolerance, and they require multiple exchanges during pregnancy, due to the potential for rapid encrustation [459].
Ureteroscopy has become a reasonable alternative in these situations [448,460]. When compared to temporary ureteral JJ stenting until after delivery, ureteroscopy resulted in reduced need for stent exchanges, less irritative lower urinary tract symptoms and better patient satisfaction [461,462].
Non-urgent ureteroscopy in pregnant women is best performed during the second trimester, by an experienced urologist. Counselling of the patient should include access to neonatal and obstetric services [78].
Although feasible, percutaneous removal of renal stones during pregnancy remains an individual decision and should be performed only in experienced centres [463]. Pregnancy remains an absolute contraindication for SWL.
3.4.14.1.1. Summary of evidence and recommendation for the management of urinary stones and related problems during pregnancy
Summary of evidence | LE |
Stent insertion seems to be more effective than conservative treatment in the management of symptomatic moderate-to-severe hydronephrosis during pregnancy. | 1a |
Ureteroscopy is a reasonable alternative to avoid long-term stenting/drainage. | 1b |
There is a higher tendency for stent encrustation during pregnancy. | 3 |
Recommendation | Strength rating |
Treat all uncomplicated cases of urolithiasis in pregnancy conservatively (except when there are clinical indications for intervention). | Strong |
3.4.14.2. Management of stones in patients with urinary diversion
Aetiology
Patients with urinary diversion are at high risk for stone formation in the renal collecting system and ureter or in the conduit or continent reservoir [464,465]. Metabolic factors (hypercalciuria, hyperoxaluria and hypocitraturia), infection with urease-producing bacteria, foreign bodies, mucus secretion, and urinary stasis are responsible for stone formation [466] (section 3.1.3). One study has shown that the risk for recurrent upper tract stones in patients with urinary diversion subjected to PNL was 63% at five years [467].
Management
Smaller upper-tract stones can be treated effectively with SWL [234,468]. In the majority of cases, endourological techniques are necessary to achieve stone-free status [232]. In individuals with long, tortuous conduits or with invisible ureter orifices, a retrograde endoscopic approach might be difficult or impossible [469].
For stones in the conduit, a trans-stomal approach can be used to remove all stone material (along with the foreign body) using standard techniques, including intracorporeal lithotripsy and flexible endoscopes. Trans-stomal manipulations in continent urinary diversion must be performed carefully to avoid disturbance of the continence mechanism [470].
Before considering any percutaneous approach in these cases, CT should be undertaken to assess the presence of overlying bowel, which could make this approach unsafe [471], and if present, an open surgical approach should be considered.
Prevention
Recurrence risk is high in these patients [467]. Metabolic evaluation and close follow-up are necessary to obtain the risk parameters for effective long-term prevention. Preventive measures include medical management of metabolic abnormalities, appropriate therapy of urinary infections, and hyperdiuresis or regular irrigation of continent reservoirs [472].
3.4.14.2.1. Summary of evidence and recommendation for the management of stones in patients with urinary diversion
Summary of evidence | LE |
The choice of access depends on the feasibility of orifice identification in the conduit or bowel reservoir. Whenever a retrograde approach is impossible, percutaneous access with antegrade ureteroscopy is the alternative. | 4 |
Recommendation | Strength rating |
Perform percutaneous lithotomy to remove large renal stones in patients with urinary diversion, as well as for ureteral stones that cannot be accessed via a retrograde approach, or that are not amenable to shock wave lithotripsy. | Strong |
3.4.14.3. Management of stones in patients with neurogenic bladder
Aetiology, clinical presentation and diagnosis
Patients with neurogenic bladder develop urinary calculi because of additional risk factors such as bacteriuria, hydronephrosis, VUR, renal scarring and lower urinary tract reconstruction [473]. The most common causes are urinary stasis and infection (Section 3.1.3). Indwelling catheters and surgical interposition of bowel segments for treatment of bladder dysfunction both facilitate UTI. Although calculi can form at any level of the urinary tract, they occur more frequently in the bladder; especially if bladder augmentation has been performed [474,475].
Diagnosis of stones may be difficult and delayed in the absence of clinical symptoms due to sensory impairment and vesico-urethral dysfunction. Difficulties in self-catheterisation should lead to suspicion of bladder calculi. Imaging studies are needed (US, CT) to confirm the clinical diagnosis prior to surgical intervention.
Management
Management of calculi in patients with neurogenic bladder is similar to that described in Section 3.3.3. In myelomeningocele patients, latex allergy is common; therefore, appropriate measures need to be taken regardless of the treatment [476]. Any surgery in these patients must be performed under general anaesthesia because of the impossibility of using spinal anaesthesia. Bone deformities often complicate positioning on the operating table [477]. The risk of stone formation after augmentation cystoplasty in immobile patients with sensory impairment can be significantly reduced by irrigation protocols [472].
For efficient long-term stone prevention in patients with neurogenic bladder, correction of the metabolic disorder, appropriate infection control, and restoration of normal storing/voiding function of the bladder are needed.
3.4.14.3.1. Summary of evidence and recommendation for the management of stones in patients with neurogenic bladder
Summary of evidence | LE |
Patients undergoing urinary diversion and/or suffering from neurogenic bladder dysfunction are at risk for recurrent stone formation. | 3 |
In myelomeningocele patients, latex allergy is common. | 2 |
Recommendation | Strength rating |
Take appropriate measures regardless of the treatment provided since in myelomeningocele patients latex allergy is common. | Strong |
3.4.14.4. Management of stones in patients with transplanted kidneys
Stones in transplanted kidneys can either be transplanted or present de novo allograft stones. Usually they are detected by routine US examination, followed by NCCT in cases of unclear diagnosis [478].
Aetiology
Transplant patients depend on their solitary kidney for renal function. Impairment causing urinary stasis/obstruction therefore requires immediate intervention or drainage of the transplanted kidney. Stones in kidney allografts have an incidence of 1% [479]. Risk factors for de novo stone formation in these patients are multi-fold:
- Immunosuppression increases the infection risk, resulting in recurrent UTIs.
- Hyper-filtration, excessively alkaline urine, renal tubular acidosis (RTA), and increased serum calcium caused by persistent tertiary hyperparathyroidism [480] are biochemical risk factors.
Management
Selecting the appropriate technique for stone removal in a transplanted kidney is difficult, although management principles are similar to those applied in other single renal units [481-483]. Additional factors such as transplant function, coagulative status, and anatomical obstacles due to the iliacal position of the organ, directly influence the surgical strategy.
For large or ureteral stones, careful percutaneous access and subsequent antegrade endoscopy are more favourable. The introduction of small flexible ureteroscopes and the holmium laser has made URS a valid treatment option for transplant calculi; however, one must be aware of potential injury to adjacent organs [482,484,485]. Retrograde access to transplanted kidneys is difficult due to the anterior location of the ureteral anastomosis, and ureteral tortuosity [486-488].Treatment of donor stones may be needed pre-transplant and increases the pool available for renal transplants. Post-transplant stone disease may also need treatment to maintain the allograft function. A systematic review evaluating the outcomes of pre- vs. post-transplant URS demonstrated a 100% SFR with an overall 7.5% complication rate, compared to SFR of 60-100% with an overall complication rate of 12.9% for post-transplant URS; most complications were Clavien 1 [489].
3.4.14.4.1. Summary of evidence and recommendation for the management of stones in patients with transplanted kidneys
Summary of evidence | LE |
Conservative treatment for small asymptomatic stones is only possible under close surveillance and in absolutely compliant patients. | 3 |
Shock wave lithotripsy for small calyceal stones is an option with minimal risk of complication, but localisation of the stone can be challenging and SFRs are poor. | 4 |
Recommendation | Strength rating |
Offer patients with transplanted kidneys, any of the contemporary management options, including shock wave lithotripsy, flexible ureteroscopy and percutaneous nephrolithotomy. | Weak |
3.4.14.5. Special problems in stone removal
Table 3.11: Special problems in stone removal
Calyceal diverticulum stones | |
Horseshoe kidneys | |
Stones in pelvic kidneys | SWL, RIRS, PNL or laparoscopic surgery [498]. |
Stones formed in a continent reservoir | Each stone must be considered and treated individually. |
Patients with obstruction of the UPJ |
|
3.4.15. Management of stones in children
The true incidence of nephrolithiasis in children remains unclear due to the global lack of large epidemiological studies. Data derived from nation-wide epidemiological studies, studies performed in different counties worldwide [504] and large-scale databases [505,506] indicate that the incidence and prevalence of paediatric urinary stone disease has increased over the last few decades. Although boys are most commonly affected in the first decade of life [507] the greatest increase in incidence has been seen in older female adolescences [504].
Stone composition is similar in children as in adults, with a predominance of calcium oxalate stones. Compared to historical data, metabolic abnormalities responsible for stone formation are less commonly identified in children nowadays [508-510]. Hypocitraturia, low urine volume and hypercalciuria predominate [87,508-510]. Age may affect the predominant metabolic abnormality with hypercalciuria and hypocitraturia being the most common disorder present in children < 10 and > 10 years old, respectively [510]. Genetic or systemic diseases (e.g., cystinuria or nephrocalcinosis) contributing to stone formation are relatively frequent in children accounting for less than 17% of the identifying causes [508,511]. The role of diet remains unclear in children, although there is some evidence that children are drinking less water and taking greater daily amounts of sodium than is recommended [512-514].
For diagnostic procedures see Section 3.3.3.2, for acute decompression see Section 3.4.2. and for metabolic evaluation see Chapter 4.
3.4.15.1. Clinical presentation
Children with urinary stones can be asymptomatic or present with non-specific symptoms that necessitate a high index of suspicion for proper diagnosis. Symptoms are age-dependent with infants presenting with crying, irritability and vomiting in 40% of cases [515] while in older children flank pain, micro or gross haematuria and recurrent UTIs are more common [516].
3.4.15.2. Conservative management
There is a lack of evidence on conservative management of paediatric stones with evidence for ureteric calculi coming from the placebo arms of medical expulsive trials, while evidence for renal stones comes from small cohort studies, either on primary stones [517,518] or residual fragments remained after SWL, RIRS or PNL [519]. Expectant management for single, asymptomatic lower-pole renal stones could be the initial approach with increased odds of stone passage, especially in patients with non-struvite, non-cystine stones < 7 mm, with no anatomic abnormalities [517]. Intervention may be needed for stones located elsewhere independently of their size [517-519].
3.4.15.3. Medical expulsive therapy in children
There are limited studies on MET as off-label expulsive therapy for children with stones which show conflicting outcomes. A systematic review of six placebo-controlled studies showed that α-blockers might increase SFR of distal ureteric stones (RR: 1.34, 95% CI: 1.16 - 1.54) [520]. A recent MA of MET for distal ureteric stones including nine RCTs found that α-blockers could significantly increase the rate of stone expulsion, reduce the stone expulsion time, decrease pain episodes and analgesia demand, but had a higher incidence of side
effects [521].
3.4.15.4. Extracorporeal shock wave lithotripsy
Shock wave lithotripsy is still the first-line treatment for most ureteral stones in children. However, it is less likely to be successful for stones > 10 mm in diameter, impacted stones, calcium oxalate monohydrate or cystine stones, or for stones in children with unfavourable anatomy and in whom localisation is difficult [522].
Studies on ESWL in children suggest an overall SFR of 70-90%, retreatment rate of 4-50% and need for auxiliary procedures in 4-12.5% of cases [523-527]. A MA of fourteen studies reporting on 1,842 paediatric patients treated with SWL found significantly higher SFR for stones < 10 mm than for stones > 10 mm and higher retreatment rates as the stone size increased [522]. For best clinical practice see Section 3.4.5. A recent MA on slow SWL vs. rapid SWL for renal stones revealed very low-quality evidence about the effects of SWL on SFRs, serious adverse events or complications of treatment and secondary procedures for residual fragments [520]. Shock wave lithotripsy is well tolerated; however, good treatment outcomes are more likely to require the administration of general anaesthesia to children. With improvements in modern (second and third generation) lithotripters, successful treatment using intravenous sedation, patient-controlled analgesia or no medication at all has been increasingly performed in a select population of older, co-operative children [528].
Based on the results of a recent MA which compared SWL to dissolution therapy for intra-renal stones, and SWL to ureteroscopy with holmium laser or pneumatic lithotripsy for renal and distal ureteric stones, no firm conclusions can be drawn about the effects of SWL on SFR, serious adverse events or complications of treatment and secondary procedures for residual fragments [520]. When SWL was compared to mPNL for lower pole renal stones 1-2 cm in size SWL resulted in lower SFRs (RR: 0.88, 95% CI: 0.80 - 0.97; moderate-quality evidence) and higher rates of secondary procedures (RR: 2.50, 95% CI: 1.01 - 6.20; low-quality evidence); however, SWL showed less severe adverse events (RR: 0.13, 95% CI: 0.02 - 0.98; low quality evidence) [529].
3.4.15.5. Endourological procedures
Rigid/semi-rigid ureteroscopy
In recent years ureteroscopy is increasingly used in children with ureteral stones [530]. Ureteroscopy proved to be effective with SFR of 81-98% [531-533], retreatment rates of 6.3%-10% [534] and complication rates of 1.9-23% [531-533,535]. Similar to adults, routine stenting is not necessary before URS. Pre-stenting may facilitate URS, increase SFR and decrease complication rates [536,537].
Flexible ureteroscopy/retrograde intrarenal surgery
Retrograde intra-renal surgery with flexible ureteroscopes (FURS) has become an efficacious treatment modality for paediatric renal stones. Recent studies report SFRs of 76-100%, retreatment rates of 0-19% and complication rates of 0-28% [538-541]. Younger age, cystine composition [542], large stone diameter [541] and lack of pre-stenting predispose to FURS failure in children [536]. A large global study across eight centres show a SFR of 75.5%; although, complications were minor, they were higher in patients < 5 years of age [543].
Although high-level evidence is lacking to support a strong recommendation [520], FURS may be a particularly effective treatment option for lower calyceal stones in the presence of unfavourable factors for SWL [533,539,544].
For large and complex kidney stones RIRS has a significantly lower SFR compared to PNL (71% vs. 95%), but is associated with less radiation exposure, lower complication rates and a shorter hospital stay [545]. Similarly, retrospectively data indicate that RIRS may achieve lower SFRs compared to minor micropercutaneous surgery in favour of shorter operative time, shorter fluoroscopy time, and less hospitalisation time [546,547]. A recently published MA confirmed these results [548].
Percutaneous nephrolithotomy
Indications for PNL in children are similar to those in adults, and include renal stones > 2 cm, or smaller stones resistant to SWL and ureteroscopic treatment. Reported SFRs with paediatric PNL are 71.4-95% after a single session [545-547,549,550] with an overall complication rate of 20% [551]. High degree of hydronephrosis, increased number of tracts and operative time [552] and large tract size [550,553-555] are associated with increased blood loss. Child age [554] and stone burden [550] predispose to the use of larger instruments during PNL in children. Miniaturisation of equipment increases the opportunity to perform tubeless PNL in appropriately selected children, which can reduce the length of hospital stay and post-operative pain [556,557]. A recent systematic review on the role of mPNL showed an initial and overall SFR of 87.9% and 97% respectively, with no conversions to standard PNL, and a complication rate of 19%, with a mean transfusion rate of 3.3% [543].
Concerns have been raised regarding possible adverse effects of PNL on the renal parenchyma of the developing child. However, focal damage is only reported in 5% of cases [558]. Using pre- and post-PNL dimercaptosuccinic acid (DMSA) scans, Cicekbilek et al. demonstrated that PNL tracts between 12-24 Charrière in size did not cause significant harm to paediatric kidneys [549].
3.4.15.6. Open and laparoscopic/robot-assisted stone surgery
With the advances in ESWL, PNL and RIRS, very few cases of paediatric urolithiasis require open surgery. Data extracted from the National Inpatient Sample (NIS) databases for 2001-2014 showed that in the USA incisional procedures (mainly nephrolithotomy, pyelolithotomy and ureterotomy) were performed in 2.6% of hospitalised patients (52% aged 15-17 years) who required surgical intervention for urinary stones [559]. Laparoscopy for the management of paediatric renal and ureteric stones is a safe and effective procedure when specific indications are followed. Stone free rates of 100% were reported when laparoscopic pyelolithotomy was applied for a > 1cm single stone located in an extra-renal pelvis [560], or when laparoscopic ureterolithotomy was applied to impacted ureteric stones > 1.5 cm, or to ureteric stones that were refractory to SWL or URS [561]. There are extremely limited data available on efficacy and complications of robot-assisted laparoscopic management of paediatric urolithiasis [562].
3.4.15.7. Special considerations on recurrence prevention
All paediatric stone formers need metabolic evaluation and recurrence prevention with respect to the detected stone type. Children are in the high-risk group for stone recurrence (See Chapter 4).
3.4.15.8. Summary of evidence and recommendations for the management of stones in children
Summary of evidence | LE |
In children, MET could increase the rate of stone expulsion, reduce the stone expulsion time, and decrease pain episodes/analgesia demand, but it has a higher incidence of side effects. | 1b |
In children, the indications for SWL, URS and PNL are similar to those in adults. | 1b |
Children with renal stones of a diameter up to 20 mm (~300 mm2) are ideal candidates for SWL. | 1b |
Ureteroscopy has become the treatment of choice for larger distal ureteral stones in children. | 1a |
In children, the indications for PNL are similar to those in adults. | 1a |
MiniPNL is safe and effective in children. | 1b |
Recommendations | Strength rating |
Offer children with single ureteral stones less than 10 mm shock wave lithotripsy (SWL) if localisation is possible or ureteroscopy as first-line option. | Strong |
Ureteroscopy is a feasible alternative for ureteral stones not amenable to SWL. | Strong |
Offer children with renal stones with a diameter of up to 20 mm (~300 mm2) SWL. | Strong |
Offer children with renal pelvic or calyceal stones with a diameter > 20 mm (~300 mm2) percutaneous nephrolithotomy. | Strong |
Retrograde renal surgery is a feasible alternative for renal stones smaller than 20 mm in all locations. | Weak |
3.5. Radiation exposure and protection during endourology
The diagnosis and treatment of nephrolithiasis is associated with high levels of ionising radiation exposure to patients [563,564]. Currently, there are no studies estimating the lifetime radiation exposure of stone formers or the subsequent risk of malignancy development. The radiation exposure of endourologists has been extensively studied. Still, there are no studies assessing the risk of radiation induced malignancies in urologists or operating theatre staff members [565-567].
Current evidence from atomic bomb patients [568,569], retrospective epidemiological data on medical exposure [570,571] and modelling studies [572,573] suggest an age and dose dependent risk of secondary malignancy from ionising radiation.
The International Commission on Radiological Protection (ICRP) recommends a maximum annual occupational exposure of 50mSv [574]. However, the risk of radiation induced malignancy follows a stochastic model having no known safe threshold of exposure. Taking this into consideration as well as the length of a urologists career the upper limit of 50mSv is still highly concerning.
Table 3.12 shows the EAU Urolithiasis guidelines panel recommended protection methods to reduce radiation exposure to patients, surgical, anaesthesiologic and nursing staff.
Table 3.12 Radiation protection measures
Limit studies or intervention involving radiation exposure to those that are strictly medically necessary. |
Implement a patient electronic record of medical imaging. |
Make use of imaging studies with lower radiation doses (US, KUB, digital tomosynthesis, low-dose and ultra-low dose CT scan). |
Create and follow a precise radiation exposure protection protocol in your department. |
Act in accordance with the as low as reasonably achievable (ALARA) principle. |
Measure and report fluoroscopy time to the operative surgeon (use dosimeters and perform monthly calculations). |
Technical measures to reduce radiation exposure include: Reducing fluoroscopy time; Limiting time adjacent to patient; Using low-dose radiation; Irradiating only to observe motion; Intra-operative use of pulsed fluoroscopy; Reduced fluoroscopy pulse rate; Collimated fields; Avoid digital image acquisition and rely on last image hold and instant replay technology. |
Use radiation protection instruments (chest, pelvic and thyroid shields, lead or lead-free gloves, protective glasses, lead protection under the operating table between the x-ray source and the surgeon). |
The radiation protection instruments must be cared for appropriately as any damage decreases effectiveness and increases exposure risk. They should be monitored and measured regularly to ensure integrity. |
Proper surgeon and operating room setup should be observed (follow the inverse square law, use the X-ray source underneath the patient’s body, decrease the X-ray source to patient distance, reduce magnification, avoid field overlap by not turning the C-arm in extreme angles, operate in the standing rather than the seated position). |
Availability of fluoroscopy is mandatory for endourological procedures. There is an increasing interest on fluoroless and fluoroscopy-free operations in urology. Several RCTs have been published showing a good outcome in means of stone free and complication rates [183,300,575-577]. These trials have been limited to non-complex cases and they were not sufficiently powered to show non-inferiority of fluoroscopy in PNL [300,565] or superiority of ultrasound in URS [249,250].