6. PROGNOSIS
6.1. Prognostic factors
Many prognostic factors have been identified and can be used to risk-stratify patients in order to decide on the most appropriate local treatment (radical vs. conservative) and discuss peri-operative systemic therapy. Factors can be divided into patient-related factors and tumour-related factors.
6.1.1. Patient-related factors
6.1.1.1. Age and gender
Older age at the time of RNU is independently associated with decreased cancer-specific survival (CSS)
[113,114] (LE: 3). Gender has no impact on prognosis of UTUC [115].
6.1.1.2. Ethnicity
One multicentre study in academic centres did not show any difference in outcomes between races [116], but U.S. population-based studies have indicated that African-American patients have worse outcomes than other ethnicities (LE: 3). Whether this is related to access to care or biological and/or patterns of care remains unknown. Another study has demonstrated differences between Chinese and American patients at presentation (risk factors, disease characteristics and predictors of adverse oncologic outcomes) [14].
6.1.1.3. Genetic pre-disposition
Patients who test positive for Lynch syndrome, based on IHC (MSI testing all 4 markers) [117].
6.1.1.4. Tobacco consumption
Being a smoker at diagnosis increases the risk for disease recurrence, mortality [118,119] and intravesical recurrence after RNU [120] (LE: 3). There is a close relationship between tobacco consumption and prognosis [121] (LE: 3); smoking cessation improves cancer control [119].
6.1.1.5. Surgical delay
A delay between diagnosis of an invasive tumour and its removal may increase the risk of disease progression. Once a decision regarding RNU has been made, the procedure should be carried out within twelve weeks, when possible [122-126] (LE: 3).
6.1.1.6. Other factors
High comorbidity and performance indices scores (e.g. American Society of Anesthesiologists [ASA], performance status [PS], and Charlson Comorbidity Index) are also associated with worse survival outcomes across disease stages [127-130].
A higher ASA score confers worse CSS after RNU [131] (LE: 3), as does poor PS [132]. Obesity and higher body mass index adversely affect cancer-specific outcomes in patients treated with RNU [133] (LE: 3), with potential differences between races [134]. Several blood-based biomarkers have been associated with locally-advanced disease and cancer-specific mortality such as high pre-treatment-derived neutrophil-lymphocyte ratio [135-138], low albumin [137,139], high C-reactive protein [137] or modified Glasgow score [140], high De Ritis ratio (aspartate transaminase/alanine transaminase) [141], altered renal function [137,142] and high fibrinogen [137,142] (LE: 3).
6.1.2. Tumour-related factors
6.1.2.1. Tumour stage and grade
The main prognostic factors are tumour stage and grade [24,104,114,143]. Upper urinary tract UCs that invade the muscle wall have a poor prognosis. In a large Dutch series of UTUC, 5-year CSS was 86% for non-muscle-invasive tumours, 70% for muscle-invasive organ-confined tumours and 44% for locally-advanced tumours [27]. A contemporary SEER analysis of RNUs for high-risk disease showed that 5-year CSS was 86% for T1N0, 77% for T2N0, 63% for T3N0 and 39% for T4N0/T any N1–3 [144]. pT3 sub staging (pT3a vs. pT3b) might be relevant [145].
6.1.2.2. Tumour location, multifocality, size and hydronephrosis
Initial location of the UTUC is a prognostic factor in some studies [146,147] (LE: 3). After adjustment for the effect of tumour stage, patients with ureteral and/or multifocal tumours seem to have a worse prognosis than patients diagnosed with renal pelvic tumours [148-153]. Hydronephrosis is associated with advanced disease and poor oncological outcome [85,94,154]. Increasing tumour size is associated with a higher risk of muscle-invasive and/or non-organ-confined disease, both in ureteral and renal pelvis UTUC. A large multi-institutional retrospective study including 932 RNUs performed for non-metastatic UTUC demonstrated that 2 cm appears to be the best cut-off in identifying patients at risk of harbouring > pT2 UTUC [155]. In a SEER database analysis of 4,657 patients with renal pelvis UTUC, each gain of 1 cm in tumour size was associated with a
1.25-fold higher risk of pT2–T4 histology at RNU [112].
6.1.2.3. Pathological subtypes
Pathological subtypes are associated with worse CSS and overall survival (OS) [68] (LE: 3). Most studied subtypes are micropapillary [71], squamous [156] and sarcomatoid [71], all of which are consistently associated with locally-advanced disease and worse outcome.
6.1.2.4. Lymph node involvement
Patients with nodal metastasis experience very poor survival after surgery [157]. Lymph node density
(cut-off 30%) and extranodal extension are powerful predictors of survival outcomes in N+ UTUC [158-160]. Lymph node dissection (LND) performed at the time of RNU allows for optimal tumour staging, although its curative role remains controversial [159,161-163] (LE: 3). Patients with clinically N+ UTUC should be offered chemotherapy, with surgery offered after a good response.
6.1.2.5. Lymphovascular invasion
Lymphovascular invasion (LVI) is present in approximately 20% of invasive UTUCs and is an independent predictor of survival [164-166]. Lymphovascular invasion status should be specifically reported in the pathological reports of all UTUC specimens [167,168] (LE: 3).
6.1.2.6. Surgical margins
Positive soft tissue surgical margin is associated with a higher disease recurrence after RNU. Pathologists should look for and report positive margins at the level of ureteral transection, bladder cuff, and around the tumour [169] (LE: 3).
6.1.2.7. Other pathological factors
Extensive tumour necrosis (> 10% of the tumour area) is an independent prognostic predictor in patients who undergo RNU [162,163] (LE: 3). In case neoadjuvant treatment was administered, pathological downstaging is associated with better OS [170,171] (LE: 3). The architecture of UTUC, as determined from pathological examination of RNU specimens, is also a strong prognosticator with sessile growth pattern being associated with worse outcome [172-174] (LE: 3). Concomitant CIS in organ-confined UTUC and a history of bladder CIS are associated with a higher risk of recurrence and cancer-specific mortality [175,176] (LE: 3). Macroscopic infiltration or invasion of peri-pelvic adipose tissue confers a higher risk of disease recurrence after RNU compared to microscopic infiltration of renal parenchyma [67,177].
6.1.3. Molecular markers
Because of the rarity of UTUC, the main limitations of molecular studies are their retrospective design and, for most studies, small sample size. None of the investigated markers have been validated yet to support their introduction in daily clinical decision making [148,178].
6.2. Risk stratification for clinical decision making
As tumour stage is difficult to assess clinically in UTUC, pre-RNU models aiming at predicting which patient has > pT2 /non-organ-confined disease have been published [179-183] (LE: 3). Several risk stratification models have been assessed with the main aim to better stratify patients eligible for kidney-sparing surgery [184-188].
Prognostic nomograms based on pre-operative factors and post-operative pathological characteristics are also available [161,181,189-194] and may be used when counselling patients regarding follow-up and administration of peri-operative chemotherapy.
As tumour stage is difficult to assess clinically in UTUC, it is useful to “risk stratify” UTUC between low- and high risk of progression to identify those patients who are more likely to benefit from kidney-sparing treatment and those who should be treated radically [184,185]. The factors to consider for risk stratification are presented in Figure 6.1.
Figure 6.1: Risk stratification of non-metastatic UTUC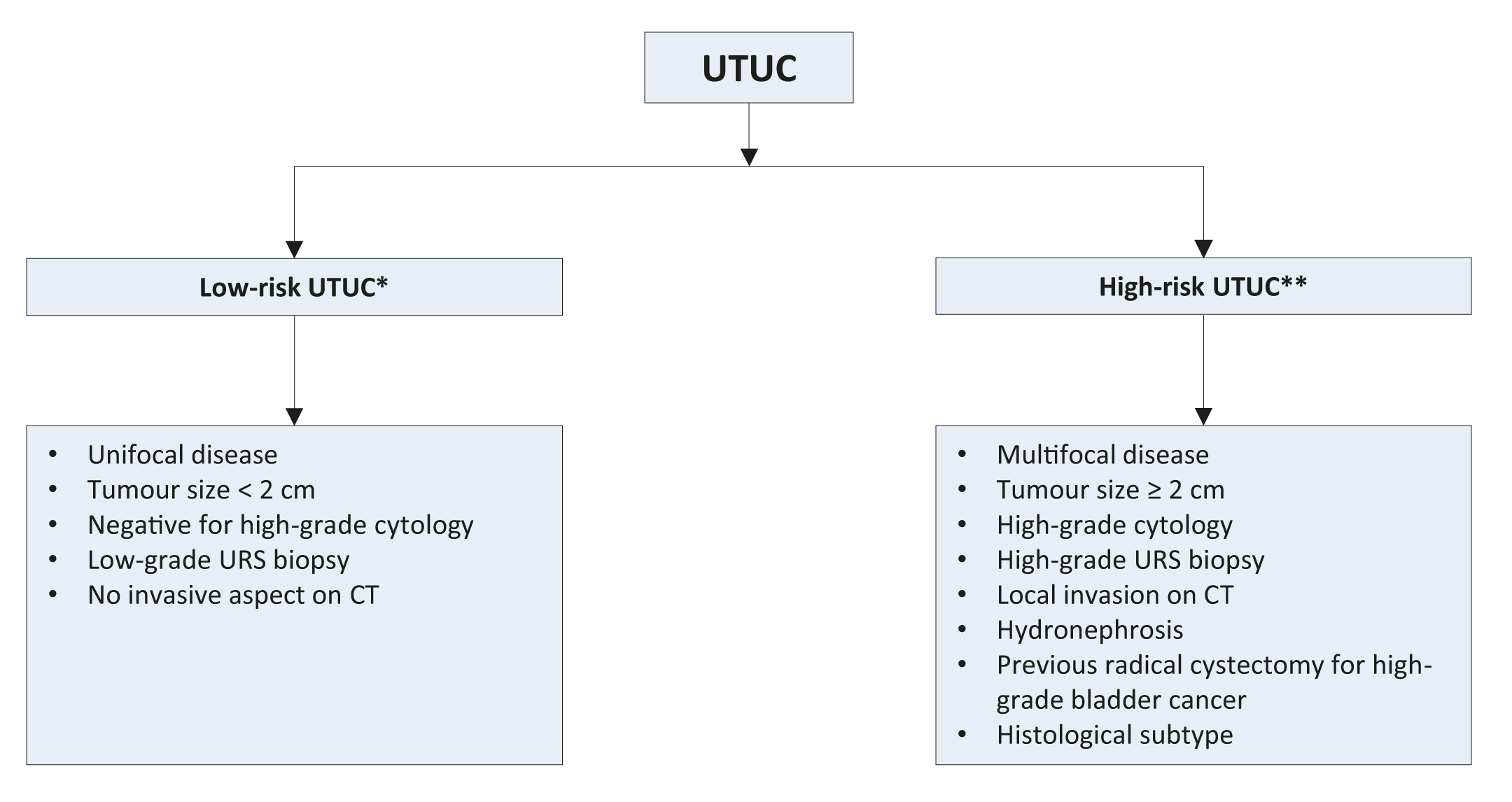 CT = computed tomography; URS = ureteroscopy; UTUC = upper urinary tract urothelial carcinoma.
CT = computed tomography; URS = ureteroscopy; UTUC = upper urinary tract urothelial carcinoma.
* All these factors need to be present.
**Any of these factors need to be present.
6.3. Bladder recurrence
A meta-analysis of available data has identified significant predictors of bladder recurrence after RNU [195]
(LE: 3). Three categories of predictors for increased risk of bladder recurrence were identified:
- Patient-specific factors such as male gender, previous BC, smoking and pre-operative chronic kidney disease..
- Tumour-specific factors such as positive pre-operative urinary cytology, tumour grade, ureteral location, multifocality, tumour diameter, invasive pT stage, and necrosis [196,197].
- Treatment-specific factors such as laparoscopic approach, extravesical bladder cuff removal, and positive surgical margins [195].
In addition, the use of diagnostic URS has been associated with a higher risk of developing bladder recurrence after RNU [198,199] (LE: 3). Based on low-level evidence only, a single dose of intravesical chemotherapy after diagnostic/therapeutic ureteroscopy of non-metastatic UTUC has been suggested to lower the rate of intravesical recurrence, similarly to that after RNU [195].
6.4. Summary of evidence and recommendation for the prognosis of UTUC
Summary of evidence | LE |
Important prognostic factors for risk stratification include tumour size, stage, grade, hydronephrosis and different histological subtypes. | 3 |
Models are available to predict pT2/non-organ confined disease and altered prognosis after RNU. | 3 |
Patient, tumour, and treatment-related factors impact risk of bladder recurrence. | 3 |
Currently, no prognostic biomarkers are validated for clinical use. | 3 |
Recommendation | Strength rating |
Use prognostic factors to risk-stratify patients for therapeutic guidance. | Weak |