9. PENILE SIZE ABNORMALITIES AND DYSMORPHOPHOBIA
Due to the demand for penile surgical procedures to enhance girth and length and the widespread use of these therapies - both medical and surgical - with very limited evidence-based data, the EAU Guidelines Panel on Sexual and Reproductive health has undertaken an extensive literature search and consensus discussion to address the issue of penile size abnormalities and dysmorphophobia. Based on the currently available evidence and the consensus of the Panel, a number of recommendations have been developed according to the invasiveness and effectiveness of the different therapeutic options. In this context, patients should be fully counselled with respect to all available treatment modalities. Most published data are derived from level 3 and 4 evidence and the vast majority of studies completely lack long-term follow-up and functional outcomes. This also includes a number of procedures which have already received formal approval from international institutions and regulatory bodies. Therefore, the strength of the recommendations in this section should be considered as a balance between data derived from low-level evidence and consensus discussions within the Guidelines Panel. As a result, a significant number of therapeutic procedures are considered exclusively experimental and should only be considered within a research setting given the potential negative effects of these procedures to patient wellbeing.
9.1. Definition, epidemiology and classification
9.1.1. History
Throughout history, the size of the penis has symbolised a marker of masculinity [1323] and has created intense debate in societies with different social and cultural implications [1324]. Indeed, along with the capacity for vaginal penetration, the penis is linked to an ancestral sense of men’s fertility and sexual performance, making the size of the penis a source of distinguishing male identity [1325,1326]. Evidence of male supremacy and dominance as represented by phallometric designs can be found across cultures and history and is still currently supported by contemporary media, including the pornographic industry [1327,1328].
Overall, cosmetic surgery has the potential to restore self-esteem, reduce anxiety, social phobia and depressive mood states regarding body concerns, increasing individuals’ well-being and quality of life (QoL) [1329,1330]. Yet, some candidates for cosmetic surgery may have psychopathological conditions and surgery may result in negative outcomes [1330,1331].
In the real-life setting, it is interesting to note that 84% women report being satisfied with their male partners’ penile size whereas 55% of the male partners were satisfied with their penile size and 45% of them report that they would like to have a larger penis [1332]. In this context, men with a high level of social-desirability were more likely than others to self-report having a larger penis [1333]. A recent study also demonstrated that reducing the depth of penetration led to a statistically significant 18% reduction of overall sexual pleasure with an average 15% reduction in length of the penis [1334].
Additionally, the subjective impression of penile size may have a negative effect on sexual functioning and QoL, impacting sexual life in about 10% of men [1335-1337]. This prevalence sharply rises in patients seeking penile augmentation procedures [1338,1339].
Furthermore, the fact that a subgroup of men does not achieve reasonable levels of satisfaction and emotional adjustment after penile augmentation procedures, underlines that with certain psychopathological conditions men will not benefit from such invasive procedures [1340]. These men may represent a psychologically vulnerable group of individuals in whom penile augmentation procedures will have negative effects and, as such, require clinical and psychological support. Clinicians should be adept to anticipate and address such vulnerability through a tailored psychological evaluation and further consider cultural standards enabling an understanding of patient expectations [1341].
With the increased use of penile augmentation procedures worldwide, either medical or surgical, it becomes crucial to create evidence-based recommendations to guide clinicians in this challenging and controversial area.
9.1.2. Definition
To date short penis condition represents both a diagnostic and treatment challenge [1342,1343]. An accurate measurement of the penile shaft is a mandatory step in the assessment of patients complaining of a short penis and defining the norm [1344]. Indeed, a standard tool to address penile measurements and to counsel patients seeking penile augmentation procedures is needed. To date, the standard penile size has yet to be clearly defined. Even though several investigators have attempted to provide objective measurements to define a normal penile size, there is still no consensus on this (Table 31).
Table 31: Summary of papers reporting objective penile measurements
Authors | Year | Patients, n | Age, years | Flaccid length, cm | Stretched length, cm | Erect length, cm | Flaccid circum-ference, cm | Erect circum-ference, cm |
Loeb [1345] | 1899 | 50; Caucasian | (17 – 35) | 9.41 | NA | NA | NA | NA |
Ajmani et al. [1346] | 1985 | 320; African - Nigeria | (17-23) | 8.19 ±0.94 | NA | NA | 8.83 ±0.02 | NA |
Schonfeld | 1942 | 54; Caucasian - USA | (20 – 25) | NA | 13.02 | NA | NA | NA |
Kinsey et al. [241] | 1948 | 2770; Caucasian | (20 – 59) | 9.7 | 16.74 | NA | NA | NA |
Bondil et al. [1348] | 1992 | 905; Caucasian - France | 53.18 ±18.19 | 10.74 ±1.84 | 16.74 ±2.29 | NA | NA | NA |
Richters et al. [1349] | 1995 | 156; Caucasian - Australia | NA | NA | NA | 15.99 | NA | NA |
Wessels et al. [1350] | 1996 | 80; Caucasian - USA | 54 | 8.85 ±2.38 | 12.45 ±2.71 | 12.89 ±2.91 | 9.71 ±1.71 | 12.30 ±1.31 |
Smith et al. [1351] | 1998 | 184; Caucasian - Australia | NA | NA | NA | 15.71 ±2.31 | NA | NA |
Bogaert et al. [1352] | 1999 | 3417; Caucasian - | 30.45 ±11.27 | 9.83 ±1.80 | NA | 15.60 ±1.88 | NA | NA |
Ponchietti | 2001 | 3300; Caucasian - | (17 - 19) | 9 (5-12) | 12.5 | NA | 10 | NA |
Schneider | 2001 | 111; Caucasian - Germany | 18.24 ±0.43 | 8.60 ±1.50 | NA | 14.48 ±1.99 | NA | NA |
Spyropoulos et al. [1355] | 2002 | 52; Caucasian - Greece | 25.9 | 7.76 | 12.18 | NA | 8.68 ±1.12 | NA |
Awwad et al. [1356] | 2005 | 271; Arab - | 44.6 | 9.3 | 13.5 | NA | 8.9 | NA |
Mehraban | 2007 | 1500; Arab - | 29.61 ±5.50 | NA | 11.58 ±1.45 | NA | 8.66 ±1.01 | NA |
Promodu et al. [1358] | 2007 | 301; Indian | 31.58 ±6.38 | 8.21 ±1.44 | 10.88 ±1.42 | 12.93 ±1.63 | 9.14 ±1.02 | 11.49 ±1.04 |
Aslan et al. [1359] | 2011 | 1132; Arab - Turkish | 20.3 ±0.9 | 9.3 ±1.3 | 13.7 ±1.6 | NA | NA | NA |
Choi et al. [1360] | 2011 | 144; oriental - Korea | 57.3 ±16.5 | 7.7 ±1.7 | 11.7 ±1.9 | NA | NA | NA |
Shalaby et al. [1361] | 2014 | 2000; African - Egypt | 31.6 | NA | 13.84 | NA | NA | NA |
Veale et al. [1342] | 2014 | 15521; Caucasian - | NA | 9.16 ±1.57 | 13.24 ±1.89 | 13.12 ±1.66 | 9.31 ±0.90 | 11.66 ±1.10 |
Habous et al. [1362] | 2015 | 778; Arab - | 43.7 | NA | NA | 14.34 ±1.86 | NA | 11.50 ±1.74 |
Hussein et al. [1363] | 2017 | 223; Arab - | 41.3 ±15 | 9.8 ±2.0 | 12.6 ±1.9 | NA | NA | NA |
Alves Barboza et al. [1364] | 2018 | Tot 627 - Brazil African 167; Caucasian 283 | 53.6 ±15 53.8 ±13.8 53.7 ±15.5 | NA NA NA | NA 16.5 ±1.7 15.8 ±1.6 | NA NA NA | NA NA NA | NA NA NA |
Di Mauro et al. [1365] | 2021 | 4685; Caucasian - | 19 | 9.47 ±2.69 | 16.78 ±2.55 | NA | 9.59 ±3.08 | 12.03 ±3.82 |
Nguyen Hoai | 2021 | 14597; Asian - Vietnam | 33.1 | 9.03 (5.10- 13.20) | 14.67 (8.30- 19.90) | NA | 8.39 (5.34-11.3) | NA |
Takure [1367] | 2021 | 271; African - Nigeria | 57.3 | 10.3 | 13.7 | NA | NA | NA |
Sole et al. [1368] | 2022 | 800; Caucasian - Argentina | 54.2 | 11.4 | 15.2 | NA | 10.1 | NA |
Measurements are expressed as median/mean, (IQR)/±SD
The other factor that strongly affects penile measurements is the interobserver variability and the underestimation of the stretched penile length (SPL) when compared to the erect state [1369].
Despite the aforementioned limitations, SPL, defined as the distance between the pubic symphysis and the apex of the glans, represents the most overlapping measurement of the erect penis. Accordingly, a SPL of less than 2.5 standard deviations (SD) below the average for a male’s age and race is considered as micropenis [1370,1371].
Summary of evidence | LE |
There is a difference between true micropenis (anatomical-endocrinological)/short penis (complaint)/buried penis (complaint short penis + obesity) (panel consensus). Small penis anxiety/syndrome refers to a man’s excessive anxiety regarding his normal-sized penis. | 4 |
A true micropenis is a congenital condition where the SPL is 2.5 SD cm less than the average length for age of the population group and is the result of an underlying genetic or endocrine condition. | 3 |
A buried penis is a normal sized penis where there is functional and visible loss of penile length due to an underlying pathological condition such as obesity or traumatic loss of length. The penis is covered by prepubic, scrotal or penile subcutaneous tissue or skin. | 3 |
Penile Dysmorphic Disorder is a shorthand concept applied to Body Dysmorphic Disorder cases characterised by a strong focus on a perceived deficiency or flaw in a normal size or shape penis, resulting in mental health impairment and significant damage in important areas of the individual’s life. | 3 |
9.1.3. Epidemiology and Classification
The overall incidence of micropenis in the male population is not clearly documented. Epidemiological studies demonstrate that between 0.015% - 0.66% of male newborns have a micropenis [1372,1373]. There are concerns that the prevalence of this congenital abnormality is increasing due to in utero exposure to endocrine-disrupting chemicals before and during pregnancy [1373]. Despite the limited prevalence of micropenis, there is a major demand for penile augmentation procedures worldwide. This phenomenon can be partially explained by the increased interest in pornography in recent years and the altered perception of a normal penile size [1324,1374,1375].
Due to the heterogeneity of clinical situations related to short penis conditions, a classification based on the underlying aetiology is provided below (Table 32).
Table 32: Classification of the clinical conditions underlying a short penis condition or dysmorphophobia in the adult
Group name | Aetiology | Definition | Pathogenesis | Prevalence, % |
False penile shortness | Acquired | Reduced exposure of the penile shaft in the presence of normal penile size | Adult acquired buried penis | NA |
Intrinsic penile shortness | Congenital | Small penis due to an incomplete genital development secondary to a congenital condition | Hypogonadotropic hypogonadism Genetic syndromes Bladder exstrophy–epispadias complex | 0.9 - 2.1 |
Intrinsic penile shortness | Acquired | Shortening/shrinking of the corpora cavernosa due to an acquired pathological process | Peyronie’s Disease Radical prostatectomy Radical cystectomy Radiation therapy Low flow priapism Multiple penile operations (e.g., urethral surgery or PP infection) Penile traumatic event (traumatic or surgical amputation for penile cancer) | NA |
Body dysmorphic disorder | Acquired | Perceived defect or flaw in the individual’s physical appearance followed by significant distress or impairment in important areas of the individual’s life | Penile Dysmorphic Disorder | 1.8 – 9.5 |
9.1.3.1. False penile shortness - congenital or acquired
Among causes underlying a false penile shortness, the buried penis is the only well-known condition. Historically, buried penis has been considered a congenital disease affecting children: the so-called “concealed penis” or “webbed penis” [1376,1377]. Indeed, an abnormal development of the dartos fascia may lead to the entrapment of the penile shaft to the peri-genital tissue leading to this clinical manifestation. On the other hand, buried penis in the adult is widely recognised as an acquired condition, termed as the adult acquired buried penis (AABP) [1378].
This condition was originally described by Dr. Keyes in 1917 [1379]. The aetiology underlying the development of AABP is deemed to be related to a chronic inflammatory state of the penile dartos which leads to a progressive retraction and scarring of the peri-genital teguments [1379,1380]. The progressive entrapment of the phallus causes a moist environment which facilitates bacterial and fungal growth causing chronic inflammation [1381]. The ensuing fibrosis results in further entrapment of the penile shaft in the peri-genital tissue [1380,1381].
Although the exact prevalence of AABP is unknown, its incidence seems to be increasing along with the growing prevalence of obesity, which represents the main risk factor for developing AABP [1382]. In Western world, up to 27.9% of the adult population have a high BMI [1382,1383]. In the last decades the overall mean waist circumference increased from 96.0 cm to 100.4 cm among men [1384]. Other factors contributing to AABP include aggressive circumcision, following surgical treatment in the obese or penile cancer (PC), or chronic dermatological conditions such as lichen sclerosis (LS) [1385]. Along with these epidemiological trends, AABP is spreading and reconstructive urologists face an increasing demand for surgical intervention.
The AABP is commonly associated with erectile and voiding dysfunctions, difficulties in maintaining adequate genital hygiene and a poor QoL [1385-1387]. A summary of risk factors for AABP and underlying issues requiring surgery is detailed in Table 33.
Table 33: Summary of studies reporting clinical characteristics of patients with AABP
Study | Year | n | Age, yr | BMI | DM (%) | HT (%) | Smoking habits (%) | History of penile cancer (%) | History of LS (%) | Underlying issues requiring surgery (%) |
Ngaage | 2021 | 15 | 53 | 37.4 ±4.3 | 7 | NR | 0 | 6 | NR | Urinary or sexual difficulties 9 (60.0%) |
Kara et al. [1389] | 2021 | 13 | 22.4 | 26 | 7% | 7% | NR | 0 | NR | Cosmetic issues 13 (100%), self-esteem/psychological well-being 13 (100%), urinary or sexual difficulties 13 (100%) |
Zhang et al. [1390] | 2020 | 26 | 33 | 29 | NR | NR | NR | NA | NR | - |
Monn et al. [1391] | 2020 | 67 | 54.76 ±12.7 | 40.4 ±6.7 | 20 (47.6%) | NR | NR | NA | NR | Urinary difficulties 50 (74.6%), pain 21(31.3%), sexual difficulties 52 (77.6%) |
Gao et al. [1392] | 2020 | 32 | 32.5 | - | NR | NR | NR | NR | NR | Cosmetic issues 32 (100%) |
Erpelding et al. [1393] | 2019 | 16 | 54 | 47.7 (25.5-53.3) | 9 | NR | 4 | NR | 2 (12.5%) | - |
Hesse et al. [1394] | 2019 | 27 | 56 | 49 | 12 (44%) | 16 | NR | NR | NR | Pain 12 (44%), sexual difficulties 8 (30%), difficulty in ambulating 9 (33%) |
Zhang et al. [1395] | 2019 | 15 | 33.2 | 28.9 ±5.3 | NR | NR | NR | 0 | NR | - |
Monn et al. [1396] | 2019 | 13 | 43.4 ±15.3 | 42.0 ±7.3 | 6 (46.2%) | NR | 4 | NR | NR | - |
Aube et al. [1397] | 2019 | 24 | 61.5 (54–67) | 38.1 (33.6–43.7) | NR | NR | 13 (54.2%) | NR | 17 (70.8%) | Personal hygiene 19 (79.2%), urinary difficulties 14 (58.3%), sexual difficulties 19 (79.2%) |
Cocci et al. [1398] | 2019 | 47 | 51.8 ±18.4 | 30 | 16 (34%) | 18 (38.29%) | NR | NR | 10 (10.63%) | Sexual difficulties 13 (27.66%), urinary difficulties 13 (27.66%), combination of urinary and sexual difficulties 12 (25.54%) |
Pariser | 2018 | 64 | 53 | 45 | 32 (50%) | NR | 16 | 0 | NR | - |
Theisen | 2018 | 16 | 48.5 | 44.7 | 9 | 9 (56%) | NR | NR | 12 (78%) | - |
Fuller et al. [1401] | 2017 | 12 | - | 45.4 ±13.8 | NR | NR | NR | NR | NR | - |
Voznesensky et al. [1402] | 2017 | 14 | 50 | 55 ±13.7 | NR | NR | NR | NR | NR | - |
Hampson et al. [1385] | 2017 | 42 | - | - | 48% | 67% | NR | 1 | 33% | Personal hygiene (67%); |
Ghanem | 2017 | 10 | 29.4 | 26.5 ±3.7 | NR | NR | NR | NR | NR | - |
Tausch | 2016 | 56 | - | 39 | NR | NR | NR | NR | NR | - |
Westerman et al. [1404] | 2015 | 15 | 51 | 42.6 (29.8-53.9) | 8 (53.3%) | NR | NR | 0 | 13 (87%) | Cosmetic issues 11 (100%), |
Rybak et al. [1405] | 2014 | 11 | 54.2 ±44.7 | 49.2 (42.4-64.5) | NR | NR | NR | 0 | 0 | - |
Shaeer | 2009 | 64 | (22-54) | - | NR | NR | NR | 0 | 0 | Cosmetic issues 64 (100%) |
Measurements are expressed as median/mean, (IQR)/±SDBMI = body mass index; DM = diabetes mellitus; HT = hypertension; LS = lichen sclerosis.
The aim of AABP treatment is to restore the functional genital anatomy and to improve QoL [1385,1386]. So far, different authors have proposed a number of classifications for AABP based upon both clinical presentation and the surgical procedure required [1378,1399].
9.1.3.2. Intrinsic penile shortness – congenital
This category encompasses the so-called “true micropenis” [1407-1409]. Despite male genital malformations being recognised as the most common birth defects, they represent a rare clinical entity with a prevalence between 0.9% and 2.1% [1410,1411]. Normal genital development is under the influence of hormonal stimulation during the fetal and pubertal periods [1412]. Several genetic syndromes may cause disturbance of the physiological hormonal axis needed for a normal genital development [1407,1413]. Even though micropenis may present as a manifestation of an endocrine or genetic disorder (most frequently hypogonadotropic hypogonadism or other genetic syndromes), it may also exist as an isolated finding without a definitive etiological cause in up to 25% of the cases [1407,1414,1415]. In particular, since placental hCG mainly regulates the Leydig cells production during gestational phase, central congenital hypogonadism does not cause disorders of sexual development. Conversely, similar to what observed for the conditions leading to development of primary or secondary hypogonadism established in the second half of gestation micro-orchidism, micropenis and cryptorchidism represent the typical clinical features in the latter cases. Finally, is should be important to recognise that the clinical model of 5-alpha reductase type 2 deficiency has better clarified that whereas T is mainly involved in the differentiation of internal genitalia, its conversion to DHT is crucial for external genitalia development [1416].The classification of the clinical conditions associated with intrinsic penile shortness in the adult is presented in Table 34.
Table 34: Classification of the clinical conditions underlying intrinsic penile shortness in the adult
Aetiology | Disturbs |
Hypogonadotropic hypogonadism |
|
Hypergonadotropic Hypogonadism |
|
Syndromic or Multiple Congenital Anomalies |
|
Unknown | - |
Amongst the pre-existing clinical entities associated with micropenis, the bladder exstrophy–epispadias complex (BEEC) is the most studied [1385,1386,1409]. It represents a spectrum of genitourinary malformations ranging in severity from epispadias to bladder exstrophy or exstrophy of the cloaca. It is considered as a rare disease, with a prevalence at birth of 1/10,000 [1407,1409,1411,1417]. It most commonly occurs as an isolated sporadic birth defect with an incidence of less than 1% [1418]. Even though surgical reconstruction aims to improve body image, this clinical entity is frequently burdened by psychosocial and psychosexual dysfunctions in the long term [1419-1425]. Additionally, male infertility is frequently associated due to poor sperm quantity or quality and hormonal impairment [1426].
9.1.3.3. Intrinsic penile shortness – acquired
This category includes a series of pathological entities that lead to the shortening of the corpora cavernosa. The different aetiologies are classified in Table 32. The mechanism underlying intrinsic penile shortening can be acute, as in the case of penile trauma or surgical amputation due to penile cancer or chronic due to a progressive fibrotic process involving the corpora cavernosa [1427-1429].
Traumatic genital injuries may commonly result from traffic accidents and gunshot wounds [1429]. Even if most of these injuries are associated with minor tissue loss, some cases may need complex genital reconstruction [1430,1431]. Rarely, a penile amputation can be the result of circumcision and genital surgical procedures such as hypospadias repair, penile prosthesis implantation or urethroplasty, and may result in a decrease in penile length [1432-1436].
Among chronic causes of penile shortening, Peyronie’s disease (PD), treatments for prostate cancer, particularly radical prostatectomy (RP) and radical cystectomy represent the most common [1338,1427,1428,1437-1445].
9.1.3.4. Body dysmorphic disorder
Body dysmorphic disorder (BDD) is a clinical diagnosis defined by the American Psychiatric Association (APA; DSM-5) as the strong distress generated by perceived defect(s) or flaw(s) in the individual’s physical appearance. This flaw is not observable to others, or, in case it exists, it appears only slightly [1446]. Over the course of this disorder, the individual has performed repetitive behaviours such as mirror checking, reassurance seeking, or mental acts such as comparing his appearance to that of others. This condition is followed by significant impairment in important areas of the individual’s social or occupational life. Individual’s concerns are not well explained by pre-occupation with body fat or weight in cases where the person’s symptoms meet the criteria for an eating disorder. Individuals presenting BDD can differ in the degree of insight, varying from good to delusional beliefs. Body dysmorphic disorder has been allocated to the Obsessive Compulsive and Related Disorders section [1446]. Muscle dysmorphia is a typology within BDD characterising individuals – usually men – with a strong pre-occupation with their perceived small muscles and body shape. Sometimes, men with BDD/muscle dysmorphia also present with an exaggerated focus on the size or shape of their penis. In those cases, Penile Dysmorphic Disorder (PDD) can be used as a shorthand concept – not listed in APA’s DSM-5 coding system. Both BDD and PDD are conceptually different from small penis anxiety (SPA) or small penis syndrome, which refers to a man’s excessive anxiety regarding his normal-sized penis. Small penis anxiety is not included under APA’s nomenclature but men with SPA may be at risk for BDD [1447]. All these definitions exclude men with true micropenis [1415,1446,1448]. Prevalence data shows that 2.2% of men in the USA and 1.8% in Germany suffer from BDD [1446]. In the military context, 9.5% of men were diagnosed with BDD and 84% reported at least some symptoms BDD [1449]. Between 3%-16% of patients undergoing cosmetic surgery are expected to present BDD, a higher rate in men (15.3%) than in women (10.9%) [1450]. However, it is worth noting that no specification regarding gender diversity has been considered in the literature; most studies seem to use a binary frame, limiting the interpretation of results. Findings on the prevalence of PDD revealed that 4.2% of men who have sex with men had PDD [1451]. No further data seems to exist on the prevalence of PDD or SPA, nor on the prevalence of BDD or PDD in the context of penile augmentation procedures.
These psychopathological entities must be differentiated from Gender Dysphoria, i.e., the clinical distress associated with the incongruence between gender identity and the gender assigned at birth; and from Koro, i.e., sudden anxiety about the penis falling back into the abdomen [1446].
9.1.4. Summary of evidence and recommendations for classification
Summary of evidence | LE |
Male genital malformations represent a rare clinical entity with an overall prevalence between 0.9% and 2.1%. | 3 |
Obesity, lichen sclerosis and penile cancer treatment are risk factors for AABP. | 4 |
Adult acquired buried penis is commonly associated with erectile and voiding dysfunctions, difficulties in maintaining adequate genital hygiene and a poor quality of life. | 3 |
Adult acquired buried penis condition can be staged upon both clinical presentation and the surgical procedure required according to available classification systems | 3 |
Bladder exstrophy–epispadias complex (BEEC) is a rare clinical condition frequently associated with male genital malformations, particularly micropenis. | 2b |
Penile traumatic or surgical amputation due to penile cancer are the most common acute causes of intrinsic penile shortening. | 3 |
The most frequent aetiologies leading to a chronic intrinsic penile shortening are PD, treatments for prostate cancer (RP, radiation therapy and androgen-deprivation therapy) and radical cystectomy. | 2b |
Body dysmorphic disorder is a clinical entity associated with a significant distress or impairment in important areas of the individual’s life. | 2b |
Penile dysmorphic disorder can be used as a shorthand concept to describe BDD patients mainly focused on penile size/shape. | 4 |
Body dysmorphic disorder/PDD can be revealed in patients requiring cosmetic surgery. | 3 |
Recommendations | Strength rating |
Perform a detailed genital examination in all men and particularly in men with BMI > 30, lichen sclerosis or penile cancer history and complaints of urinary/sexual difficulties or poor cosmesis to exclude the presence of an adult acquired buried penis (AABP) condition. | Strong |
Use classification systems to classify AABP clinical presentation and surgical management. | Weak |
Inquire on the presence of body dysmorphic disorder/penile dysmorphic disorder in patients with normal-sized penis complaining of short penile size. | Strong |
9.2. Diagnosis
9.2.1. Medical history, physical examination and psychological assessment
9.2.1.1. Medical History
The first step in the evaluation of short penis is a detailed medical history [1452]. Common causes of penile shortness should be screened and observed (e.g., history of phimosis, priapism, hypospadias/epispadias, penile trauma, penile cancer, prostate cancer, penile pain with or without acquired penile curvature suggestive of PD). A past or present diagnosis of BDD should also be noted.
9.2.1.2. Sexual history
Besides a comprehensive clinical interview with open questions regarding sexual education, development, or previous sexual experiences and fantasies, psychometric tools can be used. These include measurements of sexual functioning (e.g., The International Index of Erectile Function [IIEF]), sexual distress (e.g., The Sexual Distress Scale for men), and sexual satisfaction (e.g., Global Measure of Sexual Satisfaction) [111,1453,1454]. The propensities for sexual excitation and sexual inhibition may be further considered, (e.g., Sexual Inhibition/Sexual Excitation Scales), as well as measurements of relationship satisfaction (e.g., Global Measure of Relationship Satisfaction) [1454,1455]. Special focus should be put on the assessment of sexual performance expectations (e.g., The Dysfunctional Sexual Beliefs Questionnaire) [1456]. As a complementary assessment, body image perception can be further considered (e.g., The Body-Image Questionnaire).
9.2.1.3. Physical examination and penile size measurements
An accurate physical examination focused on the genital area is essential to the patient's initial assessment. It may reveal unsuspected diagnoses and highlight causes of congenital or acquired penile shortness. Penile abnormalities (e.g., AABP) can be disclosed on a physical inspection, and on genital palpation abnormalities (e.g., penile plaque suggestive of PD, small testis suggestive of disorders of sexual development or hypogonadism) may also be noted. The assessment of penile size and shape is mandatory to plan any subsequent medical or surgical treatment but methods for penile measurements seem to vary amongst surgeons [1344,1457]. The EAU Guidelines Panel on Sexual and Reproductive Health a SPL measurement as the bare minimum. If possible, the Panel also advocates additional measurements in both flaccid and erect state after intracavernosal injection of erectogenic agents. This is considered to be compulsory before any surgical indication. Stretched penile length can be measured both dorsally and/or ventrally from the penopubic skin junction-to-glans tip (STT) or dorsally from the pubic bone-to-glans tip (BTT) using either a measuring tape or a Vernier calliper. Overall, the measurement of penile size has not been standardised and to date there is no consensus definition due to high heterogeneity in terms of data assessment and reporting methodologies amongst different studies [1457b]. According to published data, both STT and BTT are suitable methods of measurement.
Moreover, penile girth should be noted in every patient. As for girth, both distal (coronal) and mid-shaft measurements should be recorded. Furthermore, both measures of circumference can be compared to the head-to-base ratio. The former can help classify penile shape which can be documented through photography [1458]. Although used as a surrogate, STT clearly underestimates erect penile length by about 20% [1075,1459]. Nonetheless, it is important to note that BTT seems to have a better correlation with erect penile length, especially in overweight and obese men [1075]. During physical examination it is also important to note the degree of prepubic adiposity, the status of the penile suspensory ligament and the presence or absence of a penoscrotal web.
Table 35: Penile size measurement
Length |
State Erect, stretched or flaccid Anatomic Landmarks Dorsally and/or ventrally from the penopubic skin junction-to-glans tip (STT) Dorsally from the pubic bone-to-glans tip (BTT) |
Girth |
State Erect or flaccid Anatomic Landmarks Proximal (penopubic skin junction) Middle shaft Distal (Coronal or subcoronal) |
Shape |
Head-to-base ratio Standardised photography |
9.2.1.4. Psychological assessment
A sub-group of men requesting penile augmentation procedures, usually surgery, present with strong psychological vulnerability, including BDD, or, more specifically, PDD (i.e., an excessive, pathological preoccupation with penile size or shape, despite evidence of penile normality) [1447]. This subgroup of men may be at risk for increasing psychopathology and suicide attempts and will be unlikely to achieve their surgery expectations [1460]. Currently, there is a set of freely available self-reported tools that may be used to screen patients at risk for psychopathology or poor surgical outcomes. These tools include The Body Dysmorphic Disorder Questionnaire and The Cosmetic Procedure Screening Scale for Penile Dysmorphic Disorder, screening for psychopathological cases regarding body and penile dysmorphic disorder [1447,1461]. Likewise, The Male Genital Self-Image Scale, and the Index of Male Genital Image, measuring men’s perceptions and satisfaction regarding their genitals [1462,1463]. In addition, the Beliefs About Penile Size Scale captures beliefs about the size of the penis as well as internal psychological processes [1464]. These self-reported measurements are easy to use in any clinical setting. However, evidence on BDD/PDD, further psychopathological comorbidities, and the differential diagnosis regarding personality disorders, and disorders from the obsessive-compulsive, psychotic, or emotional spectrum, should be performed by an accredited mental health expert. In addition, the subjective penile size perception should be evaluated [1340].
9.2.1.5. Counselling and outcomes assessment - Validated questionnaires
The Augmentation Phalloplasty Patient Selection and Satisfaction Inventory (APPSSI) questionnaire is a 5-item questionnaire proposed for the assessment and counselling about penile augmentation surgical treatment [1465]. The Beliefs about Penis Size (BAPS) is a 10-item questionnaire created for audit and outcome research to assess men’s beliefs about penile size [1464]. Both questionnaires have failed to correlate with penile size and lack of objective validation has restricted their use.
Despite not being specifically validated for short penile settings, other well-known self-reported psychosexual questionnaires may be considered: the IIEF-15 and the Male Sexual Health Questionnaire (MSHQ) should be administered to record baseline sexual function status and can also be used to assess its changes after treatment; the Erectile Dysfunction Inventory of Treatment Satisfaction (EDITS) can also be helpful to assess patient and partner's treatment satisfaction [111,1466,1467].
Unfortunately, these tools do not assess all the domains of this disorder focusing only on sexual/erectile function, whilst not assessing patients’ concerns and beliefs about penile size. Moreover, they have been validated only in heterosexual men.
9.2.2. Imaging
There is a lack of evidence regarding the use of imaging techniques in the assessment of patients complaining about penile shortness. Although a penile Doppler ultrasound or a penile magnetic resonance imaging may provide additional data regarding the penile anatomy and the extent of penile burying, there is no evidence that this additional information could contribute to the physical examination to justify its routine use in this clinical scenario [1344,1468-1471].
Summary of evidence | LE |
Medical/sexual history taking and physical examination are essential parts of the evaluation of men with a short penis complaint. | 4 |
Among stretched penile measurements STT may underestimate erect penile length. | 2b |
Among stretched penile measurements BTT has a better correlation with erect penile length, especially in overweight and obese men. | 2b |
Flaccid and erect state measurements to assess penile length may add useful information on penile size. | 4 |
Penile girth assessment may add useful information on penile size and shape. | 4 |
The Body Dysmorphic Disorder Questionnaire, The Cosmetic Procedure Screening Scale for Penile Dysmorphic Disorder, The Male Genital Self-Image Scale and the Index of Male Genital Image are self-reported tools useful to screen patients at risk for psychopathology. | 2b |
Mental health counselling is helpful in detecting men requesting penile augmentation procedures present with strong psychological vulnerability, including BDD/PDD. | 2b |
Validated questionnaire (e.g., APPSSI, BAPS, IIEF-15, MSHQ, EDITS) are helpful in assessing baseline sexual function and beliefs about penile size. | 4 |
Recommendations | Strength rating |
Take a comprehensive medical and sexual history in every patient presenting complaining of short penile size. | Strong |
Use stretched penile length measurements (skin junction-to-glans tip or dorsally from the pubic bone-to-glans tip) to define penile length. | Weak |
Measure flaccid and erect measurements to assess penile length in detail. | Weak |
Measure penile girth in every patient presenting complaining of a short penile size. | Weak |
Use validated questionnaires to screen for body dysmorphic disorder (BDD) in cases of a normal-sized penis. | Weak |
Use validated questionnaires (e.g., IIEF-15, BAPS) to assess baseline sexual function and beliefs concerning penile size. | Weak |
Refer patients with suspected BDD for mental health counselling. | Strong |
9.3. Management
9.3.1. Non-surgical Treatments
9.3.1.1. Psychotherapy
Penile augmentation is often motivated by the desire to improve self-perception and self-esteem [1472]. Cosmetic treatments may help increase individuals’ well-being and QoL, improving self-esteem and emotional states [1329,1330,1344]. Still, psychotherapy is recommended when psychopathological comorbidities are detected, or when aversive relationship dynamics may underly the request for penile augmentation. Addressing patients’ and partners’ motivations and expectations regarding penile augmentation seems to be a key psychotherapeutic target while no other empirical evidence is described. Poor satisfaction after penile augmentation, especially augmentation surgery, may result from the discrepancy between expected versus real penile augmentation; therefore, discussing the real morphologic changes and their long-term impact in the patients’ and partners’ subjective perceptions and sexual/relationships routines would be of paramount interest [1329,1340]. Similarly, men with BDD and SPA present a significant discrepancy between the perceived and ideal size of the penis, internalising the belief they should have a larger penis [1473]. Using a nomogram to capture the objective size, the perceived size, and the ideal size of the penis could be a useful strategy [1342]. Cognitive behaviour therapy for BDD could be applied to cases of anxiety regarding penis size, although no clinical trials have been reported [1474]. In all, it is worth noting that psychotherapy should normalise the great variability of genital shape and size [1339]. Finally, psychotherapy can be applied in the absence of a clinical/psychopathological condition; indeed, managing patient expectations could be a means to improve results and well-being associated with the surgery process.
9.3.1.2. Penile traction therapy
Despite the various surgical techniques, there are also non-invasive methods that are used to enhance penile length, including penile traction therapy (PTT) [1475]. In 2002, Colpi et al., demonstrated a +1.8 cm of penile lengthening after 4 months of use of a penile extender for at least 6 hours/day in the treatment of small penis [1476]. In a pilot phase-II prospective study that evaluated the efficacy and tolerability of a penile-extender device in the treatment of short penis, Gontero et al., used the same traction device for at least 4 hours/day for 6 months and achieved a significant gain in length, of +2.3 and +1.7 cm for the flaccid and stretched penis, respectively (both p < 0.001) [1477]. However, the change in the penile girth was not significant. In a further prospective study, these results were confirmed by Nikoobakht et al., who found a significant improvement in the mean length both for the flaccid (8.8 ± 1.2 cm to 10.5 ± 1.2 cm, P < 0.05) and the stretched state (11.5 ± 1.0 cm to 13.2 ± 1.4 cm, p < 0.05) following 3 months of use of a penile traction device [1478]. If no significant difference was found regarding proximal penile girth variation (10.5 ± 1.11 cm vs. 10.36 ± 0.69 cm, p < 0.05 ), a significant decrease in the circumference of the glans was detected (9.3 ± 0.86 cm vs. 8.8 ± 0.66 cm, p < 0.05) [1478,1479]. Again, the penile extender was instructed to be worn between 4-6 hours/day for 6 months in patients suffering from small penile length and/or girth [1479]. At 6-month follow-up, compared to baseline, a mean gain of +1.7 ± 0.8, +1.3 ± 0.4, and +1.2 ± 0.4 cm was reported for the flaccid, stretched, and erect penile lengths, respectively (p < 0.001, for all). Treatment-related side effects were rarely reported and reversible in nature, including penile numbness, pain, and bruising [1477,1478]. Treatment discontinuation rates were generally low, around 10% and mostly due to lack of efficacy, inability to comply with the treatment protocol and treatment-related side effects [1477-1479]. The broad spectrum of available PTT studies is summarised in Table 36.
Overall, PTT seems effective in lengthening the penis both in the flaccid and stretched state with minimal side effects. Yet it is not effective for penile girth enhancement. However, the quality of evidence is poor due to the lack of RCTs, and the availability of only heterogenous and small cohorts PTT has also been proven effective in the restoration of length or correction of deformities due to several diseases, including PD, or post-RP conditions [1161,1480-1482].
Table 36 : Penile traction therapy (PPT)
Author (year) | Year | n | Study design | Device | Treatment protocol | Mean age ± SD | Mean gain in penile dimensions cm (SD) |
Nowroozi | 2015 | 54 | Prospective | AndroPenis | 4-6 hours per day for 6 months | 30.1 ± 4.8 | Flaccid length: 1.7 ± 0.8 Stretched length: 1.3 ± 0.4 Erected length: 1.2 ± 0.4 |
Nikoobakht | 2011 | 23 | Prospective | Golden Erect | 4–6 hours per day during the first 2 weeks and then 9 hours per day until the end of the third month | 26.5 ± 8.1 | Flaccid length: 1.7 Stretched length: 1.71 Circumference: -0.22 Glans penis |
Gontero | 2008 | 21 | Prospective | Golden Erect | at least 4 h/day for 6 months | 45.7 ± 11.1 | Flaccid length: 2.3 Stretched length: 1.7 Circumference: NR |
NR = not reported.
9.3.1.3. Vacuum erection device
Vacuum erection devises (VED) are generally considered for patients who fail oral ED therapies [529,1452]. In contrast, data regarding the use of VEDs on penile elongation is scarce. In a study with 27 men whose SPL was <v cm, the use of a VED three times a week for 20 min on each occasion, for 6 months, did not result in a significant increase in flaccid or SPL (median values of before and after treatment of VED for SPL 7.6 cm vs. 7.9 cm, p = 0.02) [1483]. On the other hand, the benefits of using a VED following PPI and RP have been demonstrated in the literature [618,619,1483-1486].
9.3.1.4. Endocrinological therapies
Testosterone administration has been used for a long time to increase the length of the penis in infant or pre-pubertal boys with micropenis. The most common suggested dosage is 25 mg of T enanthate one a month for 3 months at the time of mini puberty, with some others authors suggesting further treatment at higher dosage at the start of [1487]. Usually this kind of approach can result in penile growth in more than 100% of cases. Topical administration of T or DHT has also been proposed by other authors with reported better outcomes with DHT, especially in poor responders to T or in those with type 2 alpha reductase deficiency [1488,1489]. Finally, the possible use of the combination of hCG and FSH treatment has also been proposed with positive outcomes [1490,1491]. Despite the treatment suggested it should be recognised that no face-to-face comparisons are available so far. In addition, long-term studies are lacking and more data are advisable to better clarify the best medical option to treat subjects with micropenis.
9.3.1.5. Summary of evidence and recommendations for the non-surgical management of short penile size
Summary of evidence | LE |
Psychotherapy should not be undertaken in the realm of preventing individuals’ legitimate choice to improve their lives. Conversely, psychotherapy is recommended when psychopathological comorbidities are detected, or when aversive relationship dynamics may underlie the request for penile augmentation. | 3 |
Cognitive behaviour therapy for BDD could be applied to cases of anxiety regarding penis size. | 3 |
Penile traction therapy proved to be an effective treatment to achieve penile lengthening. | 3 |
Vacuum erection devices proved to be an ineffective treatment in achieving penile lengthening. | 3 |
Testosterone therapy, transdermal dihydrotestosterone and recombinant gonadotropins can restore penile size in boys with micropenis or disorders of sex development. | 2b |
Testosterone therapy does not increase penile size in adult men and in men with late-onset hypogonadism. | 3 |
Recommendations | Strength rating |
Consider psychotherapy when psychopathological comorbidities are detected, or when aversive relationship dynamics may underlie the request for penile augmentation. | Strong |
Consider the use of penile traction therapy as a conservative treatment to increase penile length. | Weak |
Do not use vacuum erection devises to increase penile length. | Weak |
Use endocrinological therapies to restore penile size in boys with micropenis or disorders of sex development. | Strong |
Do not use testosterone therapy or other hormonal therapies to increase penile size in men after puberty. | Strong |
9.3.2. Surgical Treatments
9.3.2.1. Surgical treatment of adult acquired buried penis
9.3.2.1.1. Adult acquired buried penis surgical procedures classification
A broad spectrum of surgical reconstructive procedures have been proposed for AABP. According to the classification proposed by Pariser et al. different procedures may range from low complexity (including un-burying of penile shaft, reconstruction of penile shaft with the use of skin flaps or grafts, plastic surgical techniques to reconstruct the scrotum) to high complexity (including surgical removal of the suprapubic fat pad (escutcheonectomy) and operations to skin and subcutaneous fat layers of the abdominal wall (apronectomy) [1399].
The purpose of any surgical approach is to unbury the penile shaft, reconstruct genital teguments and eventually remove peri-genital or excess abdominal tissue in order to reduce the risk of recurrence. The goal is to balance an effective surgical procedure aiming to improve patient QoL, while minimising the incidence of postoperative complications. Lifestyle changes and risk factors modification, particularly weight loss, are widely considered as a proactive approach to minimise AABP surgical complications and should be encouraged before surgical intervention is undertaken. The broad spectrum of surgical interventions described to manage AABP is summarised in Table 37.
Table 37: Surgical interventions to manage adult acquired buried penis
Study | Year | n | Type of intervention (%) | Classification of |
Ngaage et al. [1388] | 2021 | 15 | 3 (20%) abdominoplasty, 5 (33%) panniculectomy, | 7 category II, 5 category IV, |
Kara et al. [1389] | 2021 | 13 | 13 (100%) circumcision, penile liberation and STSG. | 13 category II |
Zhang et al. [1390] | 2020 | 26 | 26 (100%) suprapubic liposuction and a modified Devine’s technique. | 26 category IV |
Monn et al. [1391] | 2020 | 67 | 53 (79.1%) STSG, 19 (28.4%) ligament fixation, 38 (56.7%) pubic lipectomy, 10 (14.9%) pubic liposuction, 17 (25.4%) abdominal panniculectomy, 16 (23.9%) urethroplasty. | - |
Gao et al. [1392] | 2020 | 32 | 32 (100%) suprapubic liposuction, suspensory ligament release and preputioplasty. | 32 category IV |
Aube et al. [1397] | 2019 | 24 | 17 (70.8%) STSG, 17 (70.8%) penopubic ligament fixation, 17 (70.8%) pubic lipectomy, 9 (37.5%) abdominal panniculectomy, 3 (12.5%) pubic liposuction. | - |
Cocci et al. [1398] | 2019 | 47 | (27.66%) circumcision, (19.14%) scrotoplasty, (4.25%) V-Y plasty of the pre-pubic region, (12.76%) thin STSG, (36.17%) thick STSG, (57.44%) suprapubic fat pad excision, (25.53%) abdominoplasty, (36.17%) division of suspensory ligament. | - |
Erpelding et al. [1393] | 2019 | 16 | 2 (12.5%) penile liberation and STSG, 1 (6.2%) penile liberation, STSG, eschutcheonectomy and urethroplasty, | 4 category II, 12 category IV |
Hesse et al. [1394] | 2019 | 27 | 27 (100%) Penile liberation, STSG, panniculectomy, abdominoplasty and monsplasty. | - |
Zhang et al. [1395] | 2019 | 15 | 15 (100%) suprapubic liposuction, penile suspensory ligament release and insertion of folded acellular dermal matrix between corpora cavernosa and pubis symphysis. | 15 category IV |
Monn et al. [1396] | 2019 | 13 | 6 (46.2%) penile liberation, full thickness graft to the penis using the escutcheon tissue as a graft source, 7 (53.8%) penile liberation, panniculectomy, full thickness graft to | 6 category IV, 7 category V |
Pariser et al. [1399] | 2018 | 64 | 3 (5%) penile unburying with local skin flap, 17 (27%) skin graft to the shaft, 7 (11%) scrotal surgery (scrotectomy or scrotoplasty), 33 (52%) escutcheonectomy, 4 (6%) abdominal panniculectomy. | 3 category I, 17 category II, |
Theisen et al. [1400] | 2018 | 16 | 16 (100%) escutcheonectomy, scrotectomy, and penile split- thickness skin graft. | 16 category IV |
Fuller et al. [1401] | 2017 | 12 | 12 (100%) escutcheonectomy, scrotoplasty and penile STSG. | 12 category IV |
Voznesensky et al. [1402] | 2017 | 12 | 11 (92%) debridement of penile skin and STSG to penis, 12 (100%) escutcheonectomy, 10 (83%) abdominoplasty, 7 (59%) scrotoplasty, 12 (100%) securing the supra-penile dermis to the pubic dermal or periosteal tissue. | 12 category IV/V |
Hampson et al. [1385] | 2017 | 42 | 42 (100%) limited suprapubic panniculectomy, radical excision of penile shaft skin and reconstruction with STSG and scrotoplasty if needed. | 42 category IV |
Ghanem et al. [1403] | 2017 | 10 | 10 suprapubic liposuction. | 10 category IV |
Tausch et al. [1378] | 2016 | 56 | 25 (45%) phalloplasty with or without a scrotal flap (if significant abdominal component panniculectomy to remove the excess suprapubic fat), 12 (21%) penile shaft reconstruction with STSG, 19 (34%) penile shaft reconstruction with STSG following excision of the involved tissues with any necessary adjunctive procedures. | - |
Westerman et al. [1404] | 2015 | 15 | 15 (100%) phalloplasty with ventral slit scrotal flap. | 15 category II |
Rybak et al. [1405] | 2014 | 11 | 11 (100%) penile release, 10 (90.9%) STSG. | 1 category I, 10 category II |
Shaeer et al. [1406] | 2009 | 64 | 64 (100%) adhesiolysis, suprapubic and lateral lipectomy, anchoring the penoscrotal and penopubic junctions, and skin coverage by a local flap. | 64 category IV |
The current evidence highlights the efficacy of AABP surgical treatment which has a low incidence of recurrence and satisfactory functional outcomes, as shown in Table 38, yet there is a significant incidence of post-operative complications (up to 3.5% of grade V according to Clavien-Dindo Classification) [1492].
Table 38: Surgical and functional outcomes of adult acquired buried penis repair
Study | Year | Overall post-operative complications | Recurrence of burying | Sexual outcomes | Urinary outcomes | Cosmetic outcomes |
Ngaage | 2021 | 6 (44%) | 2 (13%) | Spontaneous erections in 5 (83%) | 7 (78%) voiding in standing position | - |
Kara et al. [1389] | 2021 | 4 (30%) | - | Increase in IIEF & SSS | - | All patients were pleased with cosmetic outcome |
Zhang et al. [1390] | 2020 | 21 (80.8%) | - | - | - | Most patients had positive feedback toward their result of the operation, with the mean grade of 4.5+0.7.17 patients (65%) who were very satisfied with the outcome. Six patients (23%) were satisfied with the outcome. Three patients (12%) were neither satisfied nor dissatisfied with the outcome. None of the patients were dissatisfied nor very dissatisfied with the outcome |
Monn et al. [1391] | 2020 | 24 (57.1%) | - | 33 (49.3%) patients with erection post-operatively | - | Satisfied 25 (37.3%); unsatisfied 9 (13.4%); |
Gao et al. [1392] | 2020 | - | - | Increase in IIEF | - | - |
Aube et al. [1397] | 2019 | 15 (62.5%) | - | Good postoperative erection | - | Patients' satisfaction in case of a successful procedure was: 16 patients (76.2%) satisfied of the procedure, 5 patients (23.8%) neutral/not responding and no patients (0%) dissatisfied |
Erpelding | 2019 | 3 (18.7%) | - | - | - | - |
Hesse | 2019 | 15 (55.5%) | - | - | - | Nearly all patients (96%) reported early satisfaction with the procedure |
Zhang et al. [1395] | 2019 | 11 (73.3%) | - | No difficulty in sexual intercourses | None of patients reported difficulty in urination | 10 patients (66.7%) were very satisfied with the outcome, 4 patients (26.6%) were satisfied with the outcome, 1 patient (6.7%) was neither satisfied nor dissatisfied with the outcome, and no patient was dissatisfied with the appearance and function |
Cocci et al. [1398] | 2019 | 7 (14.9%) | - | Increase in IIEF of 3 points, vaginal penetration became possible in 97.87% of patients, erectile function improved in 42.55%, 48.93% needed to take PDE5i to enhance their nocturnal erections, improvement in penile erogenous sensation was recorded in 6.38% | - | - |
Monn et al. [1396] | 2019 | 5 (38.4%) | - | - | - | All patients reported subjective satisfaction with the cosmesis of their surgical outcome |
Pariser | 2018 | 42 (65%) | - | - | - | - |
Theisen | 2018 | 2 (10.5%) | 1 (5.2%) | Significant improvement in 10 of 13 questions (77%) | Significant improvement in 10 of 12 questions (83%) | |
Fuller et al. [1401] | 2017 | 0 (0%) | - | - | - | - |
Voznesensky et al. [1402] | 2017 | 9 (75%) | 9 (75%) | Improvement or the same degree of sexual ac- tivity (75%). | Improvement in urination (92%) | - |
Ghanem | 2017 | - | - | - | - | 3 (30%) of the patients were very satisfied with the result, 5 (50%) patients were satisfied, 1 patient (10%) was neither satisfied nor dissatisfied, and 1 (10%) patient was dissatisfied. No patients were very dissatisfied. |
Tausch | 2016 | - | - | - | - | - |
Summary of evidence | LE |
Various surgical procedures may be considered to restore genital anatomy in AABP patients. | 3 |
Acquired adult buried penis surgery is burdened by a significant incidence of postoperative complications. | 3 |
Lifestyle changes and risk factor modifications, particularly weight loss, are widely considered as a proactive approach to minimise AABP surgical complications. | 4 |
Acquired adult buried penis surgery may provide satisfactory functional outcomes with a low incidence of recurrence. | 3 |
Recommendations | Strength rating |
Extensively counsel patients on the benefits and complications of adult acquired buried penis (AABP) surgery. | Strong |
Initiate lifestyle changes and modification of risk factors, particularly weight loss, to minimise AABP surgical complications and to optimise surgical outcomes. | Strong |
Surgical reconstructive techniques may be considered to address AABP. | Weak |
9.3.2.2. Surgical treatment of congenital intrinsic penile shortness
Current literature reports a wide spectrum of possible surgical interventions aimed to address penile shortness. Nonetheless, the proposed spectrum of surgical interventions starts from less invasive procedures - such as suspensory ligament release (SLR) - to more complex genital reconstruction - such as total phallic reconstruction (TPR) [1493,1494]. These issues make the surgical treatment of congenital intrinsic penile shortness a surgical challenge in urology.
9.3.2.2.1. Suspensory ligament release
This technique involves a surgical incision and SLR of the penis which attaches the penis to the pubic bone. The surgical access is via an infrapubic incision and may be combined with an elongating V-Y skin plasty [1494]. Several authors reported outcomes of SLR in the context of a congenital intrinsic penile shortness (Table 39).
Li et al., reported the outcomes of SLR in 27 patients with PDD [1494]. The mean increase in SPL was +1.1 ± 1.1 cm, with a satisfaction rate of 27% and the request of further surgery in 54% of cases. Littara et al., conducted penile elongation in 21 patients, enlargement in 33 and combined elongation and enlargement in 301, respectively [1495]. The technique was based on penile lipofilling combined with V-Y infrapubic skin plasty and SLR. At 12 months following the surgical procedure, length at rest significantly increased from 8.8 cm to 11.4 cm, SPL significantly increased from 12.4 cm to 13.5 cm and circumference at rest significantly increased from 8.3 cm to 11.06 cm. The IIEF-5 also increased from 21.5 to 23. Similar results were reported by Zhang et al., on 15 patients [1395]. Overall, the average penile length measured pre-operatively and post-operatively was 3.0 ± 1.3 cm, 7.3 ± 2.1 cm and 5.4 ± 1.8 cm, respectively. The penile length has significantly increased by 4.3 ± 1.6 cm and 2.4 ± 0.8 cm, respectively (3 months post-operatively; p < 0.05).
Spyropoulos et al. reported on 11 psychosomatically normal men with (a) penile lengthening (suprapubic skin advancement and SLR) (n = 5); (b) penile lengthening and shaft thickening with a free dermal-fat graft shaft coverage (n = 3); and, (c) panniculectomy – suprapubic lipectomy and SLR (n = 2) [1465]. Overall, the mean penile length gain in SPL was 1.6 (1–2.3) cm, and the mean circumference gain was 2.3 cm at the base and
2.6 cm sub-coronally. Significant sexual self-esteem and functioning improvement was reported by the majority (91%) of patients.
Table 39: Suspensory ligament release
Author (year) | Year | n | Study design | Age, years | Follow up, months | Stretched penile length gain, cm |
Littara et al. [1495] | 2019 | 21 | Retrospective | 38.08 ±1.1 | 12 | 1.1 |
Zhang et al. [1395] | 2019 | 15 | Retrospective | 33.2 ± 4.6 | 3 | 4.3 ±1.6 |
Li et al. | 2006 | 27 | Retrospective | NR | 16 | 1.1 ±1.1 |
Spyropoulos | 2005 | 11 | Retrospective | 25-25 | Not reported | 1.6 (1–2.3) |
Measurements are expressed as median/mean, (IQR)/±SD.
9.3.2.2.2. Ventral phalloplasty/scrotoplasty
This intervention is based on a ventral shaft skin plasty to move the peno-scrotal angle proximally and increase the exposure of the penile shaft. Chen at al. performed ventral phalloplasty in 12 patients with satisfactory results and no complications [1496]. A longitudinal incision or Z-plasty at the penoscrotal junction, securing of the tunica albuginea to the proximal tunica dartos was performed by Xu et al., in 41 patients [1497]. Correction was successful in all patients with an improved median length of +2.1 cm in the flaccid state. Four patients experienced distal penile skin oedema, which subsided after 1-3 months without treatment. There was one recurrence in one obese patient (2.4%), on whom a second procedure was performed with good results. Yu et al., reported the outcomes of 62 patients that underwent ventral phalloplasty [1498]. A statistically significant increase in penile length of +2.6 cm was achieved for one procedure (suturing of penile shaft base to the prepubic fascia at 9 o’clock), and +2.7 cm for another procedure (suturing of penile shaft base to the prepubic fascia in the revealed state at 12 o’clock). Most patients (93.5%) were satisfied with the surgical result. No serious intra-operative or peri-operative complications were reported.
9.3.2.2.3. Suprapubic lipoplasty/liposuction/lipectomy
This intervention aims to reduce the thickness of the suprapubic fat pad either with a minimally invasive approach (liposuction) or surgically (lipectomy). The flattening of suprapubic fat pad aims to increase penile shaft exposure.
Ghanem et al., performed liposuction in ten patients using a 50-cc syringe with a 3- and 6-mm liposuction needle [1403]. The amount of fat removed ranged from 325 to 850 mL with a mean of 495.50 ± 155.39 mL. The reported complications included oedema in five patients (50%), oedema and ecchymosis in one patient (10%), oedema and hematoma in one patient (10%), while three patients (30%) did not experience complications. Three (30%) of the patients were very satisfied with the post-operative result, five (50%) patients were satisfied, one patient (10%) was neither satisfied nor dissatisfied, and one (10%) patient was dissatisfied. No patients were very dissatisfied. Shaeer’s monsplasty technique was investigated in 20 patients [1499]. Pre-operatively, flaccid visible length was 3 ± 0.9 cm, and erect visible length was 8 ±4.6 cm. At 3 months post-operatively, the flaccid visible length was 7.1 ± 2.1cm, with a 57.9% improvement in length, and erect visible length was 11.8 ± 2.1cm, with a 32% improvement in length. At final follow-up (18 months) a 73.1% improvement in satisfaction rate was detected.
9.3.2.2.4. Total phallic reconstruction
This represents the most complex genital reconstruction possible, aiming to create a new phallus with a neo-urethra. The operation is reserved for the severe penile insufficiency cases (e.g., congenital micropenis, exstrophy-epispadias complex) as benefit should be balanced over possible complications [1493].
Lumen et al., treated seven male patients (aged 15 to 42 years) with phalloplasty (6 with radial forearm free flap and 1 with anterolateral thigh flap) and implant surgery was offered approximately 1 year after the phallic reconstruction [1500]. There were no complications after surgical formation of the neophallus. Two complications were reported in the early post-operative period. Two patients developed urinary complications (stricture and/or fistula). Patient satisfaction after surgery was high in six cases and moderate in one case. Four patients underwent penile implant surgery and 50% were subsequently removed. The same group of authors performed a radial forearm free flap (RAFFF) in 7 patients and pedicled anterolateral thigh flap (ALTF) in 4 patients [1501]. There were no complications related to the flap. Aesthetic results were judged as “good” in 9 patients and “moderate” in 2 patients. Sensitivity in the RAFFF was superior compared to the ALTF. Four patients developed urinary complications (stricture and/or fistula). Six patients underwent PPI and 2 patients were explanted due to infection or erosion.
Perovic et al., conducted TPR using musculocutaneous latissimus dorsi (MLD) in 12 patients [1502]. The mean (range) follow-up was 31 (6–74) months, and the penile size was 16 (14–18) cm long and 13 (11–15) cm in circumference. There was no flap loss or partial skin necrosis.
Garaffa et al., reported a series of TPR using the radial artery forearm free flap in 16 patients with bladder/cloacal exstrophy and micropenis-epispadias complex [1503]. In one patient the distal third of the phallus was lost due to acute thrombosis of the arterial anastomosis immediately post-operatively. Almost all (93%) were fully satisfied in terms of cosmesis and size. Urethral stricture and fistula were the most common complications, which developed only at the native neourethral anastomosis. They were successfully managed by revision surgery. Sexual intercourse was achieved in 11 of the 12 patients who underwent PPI.
Harris et al., provided an update of their experience using RAFFF and ALTF phalloplasty techniques in 11 exstrophy-epispadias complex patients [1492]. A RAFFF was performed in six patients and a pedicled anterolateral thigh flap in five. Flap survival occurred in all cases and five patients subsequently received a PPI. Among patients undergoing ALTF, there was one death from acute pulmonary embolism, and the other four required at least one debulking procedure.
9.3.2.2.5. Summary of evidence and recommendations for surgical treatment of congenital intrinsic penile shortness
Summary of evidence | LE |
Considering the wide spectrum and the complexity of surgical interventions aimed to address penile shortness, this surgery should be reserved to high volume centres. | 4 |
Suspensory ligament release, ventral phalloplasty and suprapubic lipoplasty/liposuction/lipectomy provide an objective increase in penile length. | 3 |
Suspensory ligament release, ventral phalloplasty and suprapubic lipoplasty/liposuction/lipectomy are associated with a significant incidence of complications. | 3 |
Total phallic reconstruction provides satisfactory surgical and functional outcomes in men with micropenis. | 3 |
Recommendations | Strength rating |
Perform penile reconstructive surgery for adult acquired buried penis in high volume centres. | Strong |
Use suspensory ligament release (SLR), ventral phalloplasty and suprapubic lipoplasty/liposuction/lipectomy to address penile lengthening. | Weak |
Extensively discuss possible complications related to SLR, ventral phalloplasty and suprapubic lipoplasty/liposuction/lipectomy. | Strong |
Use total phallic reconstruction to restore genital anatomy in patients affected by congenital micropenis. | Weak |
9.3.2.3. Surgical treatment of acquired penile shortness
9.3.2.3.1. Penile prosthesis implantation (PPI)
The literature fails to show a direct relationship between PPI and penile length in men with ED and no concomitant PD. In a study by Deveci et al., SPL was evaluated in men undergoing primary implant surgery due to diabetes or RP [1504]. Either three-piece (Alpha-1, Mentor, USA) and two-piece implants (Ambicor, AMS, Boston Scientific, USA) were used and most patients (72%) reported a subjective decrease in penile length although no statistically significant difference was demonstrated in measured SPL. Particularly, men who had a history of RP were more likely to report subjective loss in penile length, suggesting that surgically-induced ED might be the reason for their perceived loss of length [1504]. In another study, 45 patients with PD with no deformity or penile curvature < 30° or severe penile fibrosis/scarring were implanted with an AMS 700 LGX [1505]. The mean stretched penile length improved from 13.1 ± 1.2 cm to 13.7 ± 1.1 cm and 14.2 ± 1.2 cm at 6 and 12 months, respectively. A significant difference was also observed in the length of the stretched flaccid penis between 6 and 12 months [1505]. In another study, malleable penile implantation was shown to increase penile length in a highly selected group of men with a buried penis [1506].
Apart from the studies which examined SPL in men receiving PPI, some authors have evaluated the erect penile length following PPI. In a prospective study where patients with PD were excluded, erect penile length was compared from baseline achieved by intracavernosal injection and after PPI inflation. The authors demonstrated that there were 0.83 ± 0.25, 0.75 ± 0.20 and 0.74 ± 0.15 cm decreases in erect penile length 6 weeks, 6 months, and one year post-operatively, respectively [1507]. A study where patients with PD were excluded confirmed these results as the median pre-operative pharmacologically induced length (14.25 ± 2 cm) was decreased to median post-prosthesis penile length (13.5 ± 2.13 cm) [1508]. It seems most men experience some reduction in penile length following PPI.
9.3.2.3.2. Penile disassembly
Penile disassembly has been described as a technique for penile lengthening [1509]. It basically consists of the separation of the penis into its anatomical components and inserting autologous cartilage to the space created between the glans cap and the tip of corpora cavernosa. Perovic et al., in a study with 19 patients submitted to penile disassembly and implantation of autologous rib cartilage followed by VED therapy, reported an increase of 3 cm and 3.1 cm in SPL and erect length, respectively [1509]. At a mean (range) 3.3 (1-4.5) years follow-up, the cartilaginous structures maintained their size and shape. However, in almost one third of patients, moderate dorsal penile curvature was seen, which was resolved using penile stretch and VED. The results of this surgery are poorly documented and significant complications such as glans necrosis can ensue.
9.3.2.3.3. Lengthening corporal manoeuvres
Penile length restoration with the use of the sliding technique (ST) and concomitant PPI was first described in a small series of three patients in 2012, and further supported by a larger series of 28-patient in a multi-centre study in 2015 [1316,1320]. Although this technique is only used in cases of end-stage PD with severe shortening of the shaft, 95% of men were satisfied with their increase in length with an average penile lengthening of 3.2 cm (range, 2.5-4 cm). The modified sliding technique (MoST) and multiple slit technique (MuST) are further modifications of the original ST [1317,1318]. In a series by Egydio et al., 143 patients with penile shortening and narrowing due to PD amongst other aetiologies underwent MoST or MuST procedures. The mean (range) penile length gain was 3.1 (2-7) cm at a median (range) follow-up of 9.7 (6-18) months [1317]. Recently the tunical expansion procedure (TEP) was applied in 416 patients with an average penile gain of
3.3 cm (2-6) [1318].
9.3.2.3.4. Total phallic reconstruction
The objectives of TPR are the creation of a cosmetically acceptable sensate neophallus with an integrated neourethra to allow the patient to regain urinary and ejaculatory function, followed by PPI to provide the rigidity required for penetrative sexual interaction. In general, RAFFF is the most used reconstructive approach for TPR. In a single-centre study, Falcone et al. reported their experience of 10 patients who underwent TPR using RAFFF after traumatic penile loss [1431]. The average duration between trauma and RAFFF reconstruction was 7 years. In 6 individuals, the urethral stump was sufficient for primary anastomosis and neourethra formation. The remaining patients had total penile avulsion and were voiding via a perineal urethrostomy. Consequently, a two-stage urethroplasty was necessary. Two patients developed an acute arterial thrombosis of the microsurgical anastomosis, which was successfully treated with emergency exploration. One patient had a neourethral stricture and fistula that required revision. All patients who underwent complete urethral repair were able to void and ejaculate through the phallus. After a median follow-up of 51 months, all patients were satisfied with the acquired size, cosmesis, and sensation. Six patients received a PPI and were able to also engage in penetrative intercourses. However, three patients had revision surgery (2 due to infection and 1 due to mechanical failure) [1431].
9.3.2.3.5. Summary of evidence and recommendations for surgical treatment of acquired penile shortness
Summary of evidence | LE |
Penile prosthesis implantation is not effective in increasing penile length. | 3 |
The evidence for the use of penile disassembly manoeuvres and the sliding technique are limited. | 3 |
Total phallic reconstruction yields to satisfactory outcomes despite the high incidence of post-operative complications. | 3 |
Recommendations | Strength rating |
Do not recommend penile prosthesis implantation, penile disassembly or sliding technique to patients seeking penile lengthening options. | Strong |
Use total phallic reconstruction to restore genital anatomy in genetic males with penile inadequacy due to traumatic loss. | Weak |
9.3.2.4. Penile Girth enhancement
9.3.2.4.1. Penile Girth enhancement history
Mean flaccid penis circumference is 9.31 cm (± 0.90 cm), and the erect penile circumference is 11.66 ±
1.10 cm [1342]. Unlike penile lengthening, there are no precise definitions or indications for penile girth enlargement in the literature or existing international guidelines [1510]. In recent years, men have increasingly approached urologists for penile girth enhancement to increase their self-confidence, to be cosmetically satisfied or to satisfy their partners [1511]. In recent surveys, it has been reported that the diameter of the penis is more important for orgasm in women than the length of the penis and actually 84% of women are satisfied with their partner’s penis size [1512,1513]. On the other hand, no valuable data are available for men who have sex with men. Current reports on penile girth enhancement techniques are from recent years [1511,1514]. Although these surgical techniques are more and more frequently requested, the level of evidence for their use in clinical practice is low, notwithstanding the ethical considerations of surgery in this vulnerable group of patients.
9.3.2.4.2. Injection therapy
Injectable filling materials can be classified according to their different properties. They can be autologous, biological or synthetic in nature. The fat injection material is obtained from the patient’s own tissue (autologous), usually by liposuction (see the following surgical therapy section). Biological fillers can be of human and animal (collagen) or bacterial (Hyaluronic acid) origin. Poly-l-lactic acid (PLA), hydroxyethyl methacrylate, polyalkylimide hydrogel (PAAG), polymethylmethacrylate (PMMA), calcium hydroxyapatite (CHA), silicon and paraffin constitute filler materials of synthetic origin (Table 40) [1515].
Table 40: Origin of injectable filling materials
Origin of injectable filling materials | |
Autologous | Autologous fat tissue |
Biological | Hyaluronic acid |
Synthetic | Poly-l-lactic acid, hydroxyethyl methacrylate, polyalkylamide hydrogel, polymethylmethacrylate, calcium hydroxyapatite, silicon, paraffin |
9.3.2.4.2.1. Soft tissue fillers (Hyaluronic acid and PMMA)
Hyaluronic acid
Injection of hyaluronic acid (HA) gel is one of the most commonly used injectable fillers in the field of plastic surgery [1452,1516]. The application of HA for penile girth enhancement has recently gained increasing popularity due to its biocompatibility and infrequent mild temporary side effects. The newly invented cross-linked HA has a more lasting effect over time [1517]. Hyaluronic acid has been used for patients for penile girth enhancement. Studies have reported that an increase of 1.4 to 3.78 cm in penile girth is achieved with HA injection (Table 41). Patient satisfaction is high (78-100%) and no severe side effects have been reported
[895,1518-1521].
Table 41: Published data on evaluation of Hyaluronic acid injection therapy on penile girth enhancement
Author | Year | n | Study design | Age, years | Follow-up, months | Girth gain, cm | Complications, n (%) |
Zhang et al. [1522] | 2022 | 38 | Retrospective | 31.2 ± 6.7 | 12 | 2.44 ± 1.14 | 3 (7.9) |
Ahn et al. | 2021 | 32 | Multi-centre RCT | 20-65 | 5-6 | 2.27± 1.26 | 2 (6.3) |
Quan et al. [1523] | 2021 | 230 | Retrospective | 30.34±5.23 | 6 | 1.80 ± 0.83 | 10 (4.3) |
Yang et al. [1520] | 2020 | 39 | Multi-centre RT | 19-65 | 5-6 | 2.1 ± 1.0 | 2 (5.13) |
Yang et al. [1521] | 2020 | 33 | Multi-centre RT | 20-66 | 18 | 1.41 ± 1.48 | 3 (9.1) |
Yang et al. [1518] | 2019 | 36 | Multi-centre RT | 20-65 | 11-12 | 1.69 ± 1.53 | 1 (2.78) |
Kwak et al. [1519] | 2011 | 50 | Retrospective | 42.5 (27-61) | 18 | 3.78 ± 0.35 | 0 (0) |
Summary | N/A | N/A | 19-66 | 5-18 | 1.40 – 3.78 | 0-9.1 |
Measurements are expressed as median/mean, (IQR)/±SD.
Polymethylmethacrylate (PMMA)
Polymethylmethacrylate (PMMA) microspheres have been injected as a wrinkle filler. An average increase in penile circumference of 3.5 cm was reported in two studies using PMMA for penile girth enhancement [1524,1525]. The authors reported that post-operative swelling and inflammatory reaction resolved within a few days and no pattern of PMMA microspheres migration to neighbouring regions was seen.
Poly-l-lactic acid
Poly-l-lactic acid (PLA) is another widely used soft tissue filler. Poly-l-lactic acid has enhanced effects by stimulating fibroblast proliferation and increasing collagen deposition in tissue. An average increase of 1.2 to 2.4 cm has been reported in the penile girth with PLA injection. No complications other than temporary local pain and swelling were reported in the treated patients [1518,1526].
9.3.2.4.2.2. Other Fillers (silicone, paraffin)
Foreign body injections are still frequently practiced in many countries (especially in east Asia and east Europe), either by the patient himself or by healthcare workers, using various substances such as paraffin, silicone or petroleum jelly (Vaseline), to increase the circumference of the penis [1527]. This results in a chronic granulomatous inflammatory foreign body reaction [1527,1528]. The result of this practice is a pathological condition called sclerosing lipogranuloma of the penis also referred as paraffinoma or siliconoma according to the substance used [1527]. The resultant inflammatory process ranges from oedema and infection to Fournier’s gangrene. Penile reconstructive surgeries may be required when siliconoma and paraffinoma require excision [1527-1533].
9.3.2.4.3. Surgical therapy
9.3.2.4.3.1. Autologous fat injection
This is a surgical technique based upon thinning the lower abdomen with liposuction and injecting the harvested fat tissue into the penile shaft [1534-1537]. The liposuction technique is performed by making two 2-3 mm long incisions from the medial side of both anterior superior iliac spines and by irrigation of 500-1,000 cc
saline containing lidocaine and adrenaline to lower abdominal subcutaneous fat tissue. Approximately 40–80 mL
of fat is extracted from lower abdomen. After centrifugation, the adipose tissue is separated from the serum and made ready for injection. In retrospective studies, an average increase of 2 to 3.5 cm in penile circumference was reported in patients who underwent autologous fat injection. No statistically significant decrease was observed in IIEF scores and no serious adverse events, such as penile abscess or deformity requiring reoperation occurred. Post-operative satisfaction survey showed that more than 75% of patients were satisfied. RCTs with high level of evidence and long-term outcomes are needed to validate such surgery
(Table 42) [1495,1534,1535,1538].
Table 42: Published data on evaluation of autologous fat injection on penile girth enhancement
Author (year) | Year | n | Study design | Age (years) | Follow up (months) | Girth gain (cm) | Complications, n (%) |
Littara et al. [1495] | 2019 | 334 | Retrospective | 36 | 12 | 2.76 | 49 (14.67) |
Salem et al. [1538] | 2019 | 15 | Prospective | 33 (23-45) | 6 | 2-3.5 | N/A |
Kang et al. [1534] | 2012 | 52 | Retrospective | 42.1 | 6 | 2.18-2.28 | 1 (1.92) |
Panfilov et al. [1535] | 2006 | 60 | Retrospective | 33.8 | 12 | 2.65 | 3 (5) |
Summary | N/A | N/A | N/A | 33-42.1 | 6-12 | 2-3.5 | 1.92-14.67 |
Measurements are expressed as median/mean, (IQR)/±SD.
9.3.2.4.3.2. Grafting procedures (albugineal and peri-cavernosal)
Surgical techniques using grafts for penile girth enhancement are controversial. Until more rigorous multi-institutional studies reporting on complications and validated outcomes are known, penile girth enhancement procedures using grafts should be considered experimental (Table 43).
In a study of 69 patients using the porcine dermal acellular matrix graft (InteXen; American Medical Systems, Minnetonka, MN, USA) a 3.2 cm increase in flaccid state and 2.4 cm in erect state was reported at one year following surgery. The procedure was performed with an infrapubic incision, and 68 of 69 patients reported significant satisfaction using the Augmentation Phalloplasty Patient Selection and Satisfaction Inventory. Graft fibrosis has been observed in up to 13% of patients, and a mean reduction in penile length of 0.5 cm has been reported in patients with fibrosis [1539]. In a study performed in 18 patients treated with acellular collagen matrix graft (Pelvicol; CR Bard, Inc., Covington, GA, USA), only 2 patients reported satisfaction, and graft removal was required in 4 patients and penile hypoesthesia in 4 patients [1540].
Techniques using venous grafts for penile girth enhancement have also been described [1541]. Initial results are encouraging, but better designed RCTs are needed.
Dermal fat grafts are free onlay grafts composed of deepithelialized dermis and subcutaneous fat. An area of approximately 10 x 5 cm is required for graft harvesting. An increase in penile girth of 1.67 to 2.3 cm has been reported in studies with the dermal fat graft technique. Penile oedema up to 27%, painful erection up to 27%, and curvature due to graft fibrosis up to 9% have been reported. Side effects such as penile hypoesthesia, skin necrosis, and infection were not reported [1465,1542,1543]. In a study involving 30 patients who underwent dermal graft combined with SLR for penile enhancement, it was reported that an increase of 1.5 cm in the flaccid phase and an average increase of 1.2 cm in the erect state on penile girth was achieved. Mean age was 23.7 (19-35) years and the mean follow-up period was 13 months. Penile oedema in seven patients and local skin necrosis in one patient were reported [1544].
Table 43: Published data on evaluation of grafting techniques on penile girth enhancement
Author (year) | Year | n | Study design | Technique | Age, years | Follow up (months) | Girth gain (cm) | Complications, n (%) |
Elist et al. | 2018 | 400 | Retrospective | Subcutaneous silicone implant | 35 | 48 | 4.9 | 86 (21.5) |
Zhang et al. [1544] | 2016 | 30 | Retrospective | Dermal graft | 23.7 | 13 | 1.5 | 1 (3.3) |
Xu et al. | 2016 | 23 | Retrospective | SLR + skin advancement + dermal fat graft | 23 | 6 | 1.67 | 7 (30.43) |
Tealab et al. [1540] | 2013 | 18 | Retrospective | Acellular collagen matrix graft | 24 | 12 | 2.3 | 8 (44.44) |
Mertziatis | 2013 | 82 | Retrospective | SLR + skin advancement + Dermal fat graft | 24 | 12 | 2.2 | 25 (31.64) |
Spyropoulos | 2005 | 4 | Retrospective | SLR + Dermal | 32 | 14 | 2.3 | No major complication |
Alei et al. | 2012 | 69 | Retrospective | Porcine dermal acellular matrix graft | 28.2 | 12 | Flaccid: 3.2; | 19 (27.5) |
Austoni et al. [1541] | 2002 | 39 | Retrospective | Corporal venous graft | 24-47 | 9 | Flaccid: | 1 (2.56) |
Summary | N/A | N/A | N/A | N/A | 18-68 | 6-48 | 0-4.9 | 0-44.44% |
9.3.2.4.3.3. Biodegradable scaffolds
This is a technique based on using fibroblasts (harvested from patients’ own scrotum skin and dartos tissue) in tissue cultures and seeding them in microporous biodegradable poly-lacti-co-glycolic acid (PLGA) scaffolds and implanting these scaffolds between Dartos and Buck’s fascia. A limited number of studies have reported girth gain of up to 4.02 cm with implantation of biodegradable scaffolds [1546-1548] (Table 44).
Table 44: Published data on evaluation of implantation of biodegradable scaffolds
Author | Year | n | Study design | Age (years) | Follow up (months) | Girth gain (cm) | Complications, n (%) |
Djordjevic et al. [1546] | 2018 | 21 | Retrospective | 28 (22-37) | 38 (13-66) | Flaccid: 1.1 ± 0.4; Erect: 1±0.3 | 2 (9.52) |
Jin et al. [1547] | 2011 | 69 | Multi-centre non- controlled | 33±9.14 | 6 | Flaccid: 4.01; Erect: 4.02 | 6 (8.69) |
Perovic et al. [1548] | 2006 | 84 | Multi-centre prospective non- controlled | 28.77±6.61 | 24.67 | Flaccid: 3.35; Erect: 2.47 | 8 (9.52) |
Summary | N/A | N/A | N/A | 18-60 | 6-60 | 1-4.02 | 8.69-9.52% |
9.3.2.4.3.4. Subcutaneous penile implant
Recently, a silicone penile implant called “Penuma®” (International Medical Devices [Beverly Hills, CA, USA]) has been approved and has shown promising results for penile girth enhancement. Penuma® is a soft silicone subcutaneous implant placed on 3/4 of the penile shaft and fixed to the glans with a polyester mesh [1545]. Studies have reported an average increase in penile circumference of 2 to 5 cm with Penuma® insertion. According to published data complication rates (usually mild and transient, occur in <5%) and the removal rate (1%) of the implant has been reported to be relatively low [1545,1549].
9.3.2.4.4. Summary of evidence and recommendations for penile girth enhancement
Summary of evidence | LE |
Various surgical approaches with specific outcomes and complications have been considered to address penile girth enhancement, with limited benefit. | 3 |
Hyaluronic acid (HA), Poly-l-lactic acid (PLA), hydroxyethyl methacrylate, polyalkylamide hydrogel (PAAG), polymethylmethacrylate (PMMA), calcium hydroxyapatite are used as injectable materials for penile girth enhancement. | 3 |
Patient satisfaction with soft tissue fillers (especially HA, PMMA and PLA) is high (> 78%). | 3 |
No complications other than temporary local pain and swelling were reported in patients treated with soft tissue fillers. | 3 |
Using silicone, paraffin and petroleum jelly (Vaseline) in penile girth enhancement causes a range of complications ranging from oedema to infection to Fournier’s gangrene. | 3 |
Not enough long-term data are available on autologous fat injection for penile girth enhancement. | 4 |
Not enough long-term data are available on grafting procedures (dermal acellular matrix graft, venous grafts or dermal fat grafts). | 4 |
Grafting procedures are associated with a high complication rate and low rate of patient’s satisfaction. | 3 |
Not enough long term data are available on biodegradable scaffolds and subcutaneous penile implant (Penuma®) . | 4 |
Recommendations | Strength rating |
Counsel patients extensively regarding the risks and benefits of penile girth enhancement techniques. | Strong |
Do not use silicone, paraffin and petroleum jelly (Vaseline) to address penile girth enhancement. | Strong |
Use hyaluronic acid, soft tissue fillers and autologous fat injection to address penile girth enhancement. | Weak |
Do not use hyaluronic acid, soft tissue fillers and autologous fat injection to address penile girth enhancement in men with penile dysmorphic disorder. | Weak |
Do not use grafts in penile girth enhancement as they are considered experimental. | Strong |
Do not use biodegradable scaffolds and subcutaneous penile implant (Penuma®) to address penile girth enhancement as they are considered experimental. | Strong |
Figure 12: Management of short penile size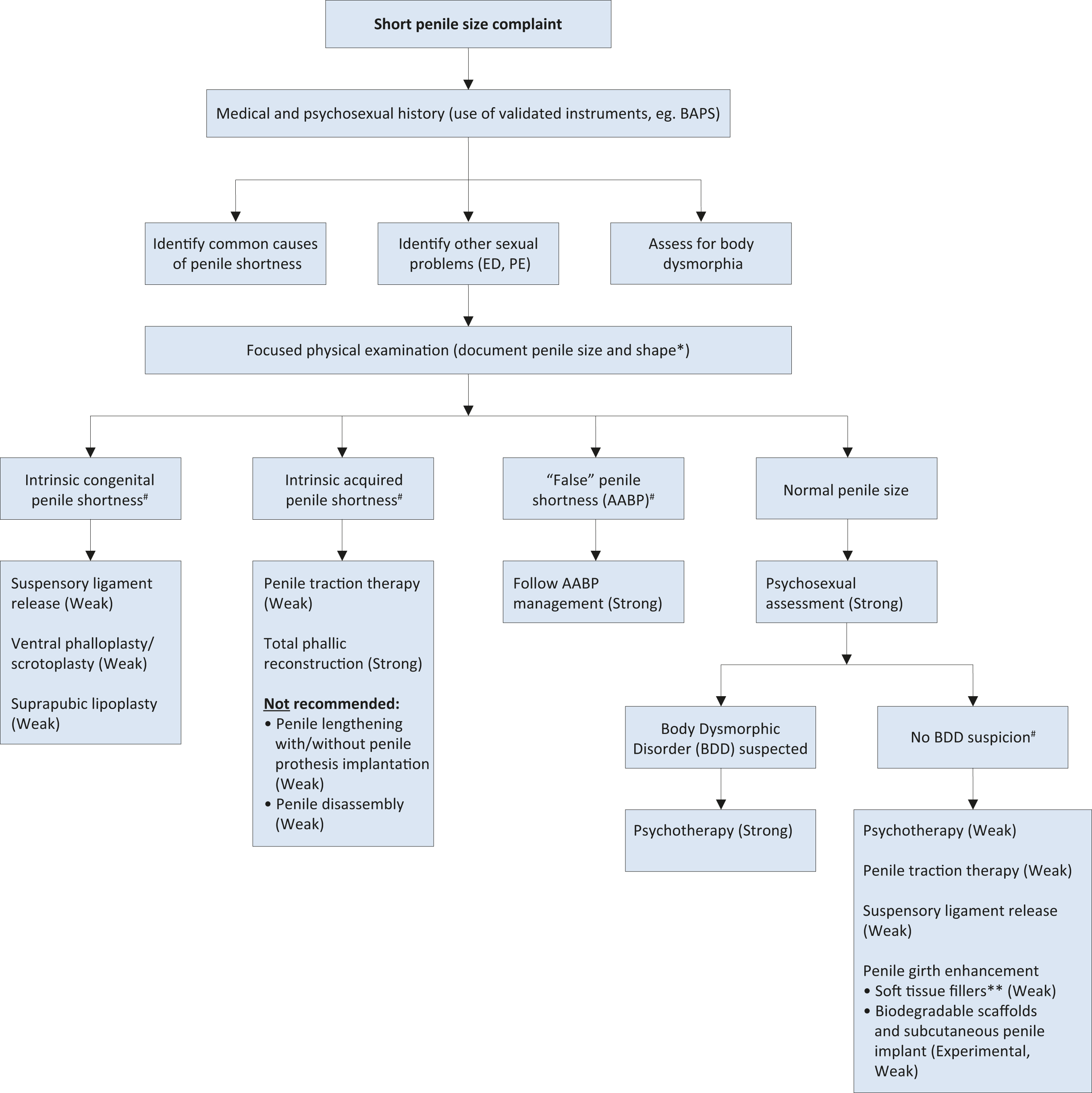 * Penile length should be measured stretched both from penopubic skin junction-to-glans tip (STT) and from the pubic bone-to-glans tip (BTT).
* Penile length should be measured stretched both from penopubic skin junction-to-glans tip (STT) and from the pubic bone-to-glans tip (BTT).
# There is lack of evidence to recommend one treatment over another.
**Hyaluronic acid (HA), poly-l-lactic acid (PLA), hydroxyethyl methacrylate, polymethylmethacrylate (PMMA), polyalkylamide hydrogel (PAAG) and calcium hydroxyapatite are considered as injectable materials for penile girth enhancement. Although the level of evidence is low, there is more evidence for HA, PLA and PMMA. Do not use silicone, paraffin or Vaseline (Strong evidence against).
Strength of recommendations is depicted between brackets where appropriate.
9.3.2.5. Functional outcomes: sexual function, sensitivity, impact on quality of life and emotional adjustment
Cosmetic treatments, including surgery, help to restore self-esteem, reduce anxiety, social phobia, and depressive mood states regarding body concerns, increasing individuals’ well-being and QoL [1329,1330]. Therefore, we can expect men with genuine short penis to use available resources to adjust the length or girth of their penis as a mean to improve their sense of identity and fit cultural standards regarding penile size and function. Men who pursue penile augmentation report being motivated by the desire to improve self-perception and self-esteem [1328,1339] (which are legitimate goals), and connect penile augmentation to a psychological need rather than an exclusive physical or functional requirement. Currently, the results of penile augmentation techniques seem mixed. The use of fillers resulted in improved genital self-image and self-esteem, lower PDD symptoms, but no effects were found regarding self-confidence or sexual relationship satisfaction [1472]. Likewise, penile lengthening or girth enhancement surgery seem to result in poor satisfaction, poor erectile function and sensitivity in men with normal penis size [1340]. Despite those negative outcomes, cases of increased satisfaction have been registered [1550]. Male genital self-image has been related to IIEF domains: sexual desire, orgasmic and erectile function, intercourse and overall satisfaction [1462]. Similarly, perceived penis size seems to predict erectile function more than objective size [1336]. In addition, reduced penetrative and receptive oral sex are associated with men’s dissatisfaction regarding their penis [1551]. For these reasons, more efforts should be made in order to clarify the impact of penile augmentation treatments on men’s and partners’ well-being and QoL. As for men with BDD, they have shown reduced erectile and orgasmic function, as well as less intercourse satisfaction as compared with controls, while men with SPA revealed reduced satisfaction. Sexual desire seemed untouched in BDD and SPA cases [1472,1552].
9.3.2.6. Ethics
Evidence regarding the medical and psychological context of penile augmentation is lacking. However, existing data suggest that motivations for penile augmentation may be strongly connected to psychological rather than physical needs. Influence of pornography, comparison with peers, and appearance-related teasing, have been reported as motives for pursuing penile augmentation [1328]. Furthermore, some treatment candidates, particularly candidates for penile cosmetic surgery, may present an underlying psychopathological condition such as BDD, which predicts poor surgical outcomes. Within this regard, the decision to implement penile augmentation techniques becomes an ethical issue.
Usually, when exploring medical ethics, we take into account several principles representing different dimensions that should be explored in medical decision-making [1553]. These include personal, clinical and social dimensions that should be considered to help doctors make ethical choices. It is clear for us that a medical decision should be taken together with doctors and patients, reaching an agreement considering the patient's will, the foreseeable clinical consequences (including psychological) and any social (fair decisions, interests of third parties) and consequences of reliance on professionals.
Respect for self-determination is central to current medical ethics. The individual diversity of the human being is increasingly marked, and it is more and more difficult to define the best interest of the patient solely cantered on clinical dimensions. The perception of illness vs. health is less and less dichotomous. In that sense, the main objective of medicine should be considered in terms of the patient well-being, which makes medical decisions increasingly dependent on subjective dimensions.
In the context of an intervention such as penile augmentation the personal dimensions are central. On the one hand, people with micropenis and consequent functional difficulties should be able to benefit from surgical On the other, people with BDD should be referred for psychological and/or psychiatric interventions, which are the first-line therapies for this disorder. Doctors and their patients must consider psychological counselling prior to reaching a decision. Patients’ motivations, discussions of potential positive and negative outcomes, and the opinions of sexual partners guide the patient and his doctor to reach an informed, ethical decision to improve satisfaction.
Clinicians will always have the first and last word in deciding treatment. In cases where the diagnosis is clear, they may proceed to intervention. Whenever the circumstances raise some doubts, they may refer the patient for counselling. Finally, they may veto the intervention whenever they believe it could be harmful to the patient, such as in cases where the diagnosis of BDD is clear, referring the patient for psychological assessment.
Social issues are always more complex but should still be considered. Should health insurance or the National Health Service include these interventions in their basic packages? And can they do so without a clearly identified diagnosis? The truth is that these issues can generate great suffering for people, but the central question is whether, in a context of scarcity of resources, a prioritisation of resources is mandatory. In the wider context; what level of priority should be given to penile augmentation surgery. Whilst the clinician must be focused on treating the patient consideration must be given to the effectiveness of surgery in this setting.
Finally, the issue of professional responsibility - i.e., the responsibility that all doctors have to reinforce public confidence in medical practice - as an activity that aims not only to provide a service, but to promote the best interest of the patient and considering the patients’ health. It should be taken into consideration that, at this level, it is important that interventions reinforce people's trust in doctors. Therefore, exploring the various dimensions of their health (including the psychological dimensions), may be much more reinforcing of this trust than simply complying with patients' requests and providing immediate satisfaction with a surgical intervention. Therefore a full and informed discussion of the possible consequences and management of unrealistic expectation must be undertaken with the patient.
While existing techniques have some success at achieving penile augmentation or enhancement, they do not guarantee positive outcomes in terms of psychological adjustment. Indeed, they may actually impact on pre-existing psychological vulnerabilities. There is evidence that a number of men receiving counselling do not proceed with surgery [1554]. Accordingly, it is advisable that the patient and his/her partner receive psychological/psychiatric feedback on potential underlying psychopathology; in case the patient proceeds to surgery, managing the patient’s and partner’s expectations regarding the long-term impact of the surgery or any type of treatment should be a priority. Given the current scenario, a multi-disciplinary team may offer the patient a treatment approach that is sensitive to patient needs, ethical standards and does not compromise the patient’s mental health. An open doctor-patient communication regarding expectations, specific risks, benefits, and alternatives is paramount to facilitate better results in this complicated field.
9.3.2.7. Final remarks
The complaint of “short penis” is variable in presentation and aetiology. Some patients demonstrate anatomical and pathological conditions while others do not. A vast array of treatments for different aetiologies of “short penis,” both surgical and non-surgical, have been reviewed. If psychopathological symptoms are detected, the patient must be referred for further medical diagnosis. Treatment for short-penis syndrome requires a multi-disciplinary approach, including medical and ethical considerations, and the majority of reported outcomes are based on a paucity of evidence. Specifically, care providers are strongly advised to counsel patients about the advantages and disadvantages of penile augmentation procedures before recommending irreversible treatments with limited evidence base.